The document outlines the Curriculum Implementation Support Program (CISP) developed by the Medical Council of India to provide intellectual support to medical colleges for a smooth transition from the existing to the new competency-based undergraduate medical education curriculum. The CISP will be conducted through workshops at Nodal and Regional centers focusing on areas like foundation course, early clinical exposure, integrated teaching and learning, and skill development and training. The program aims to build the capacity of faculty so they can effectively implement the revised curriculum.























![31
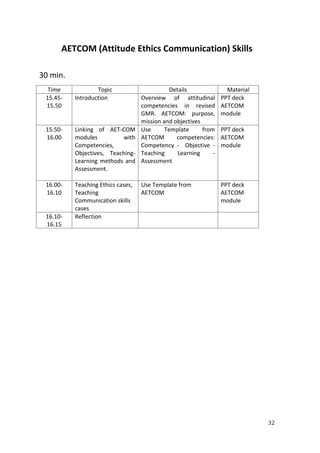
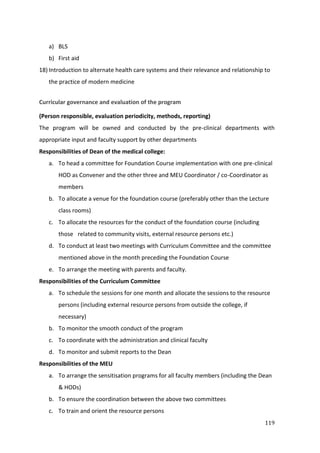
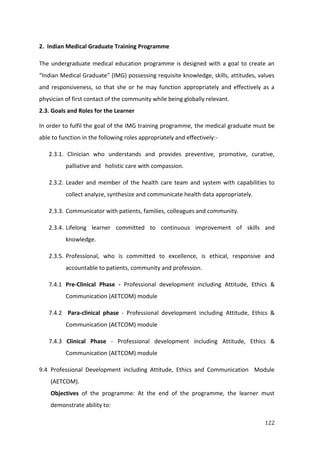
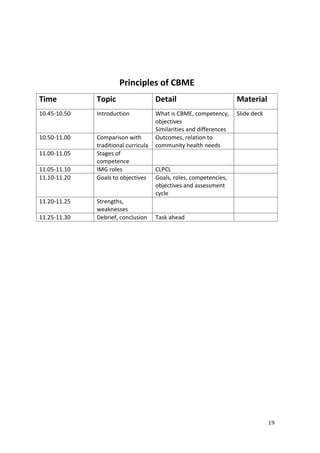
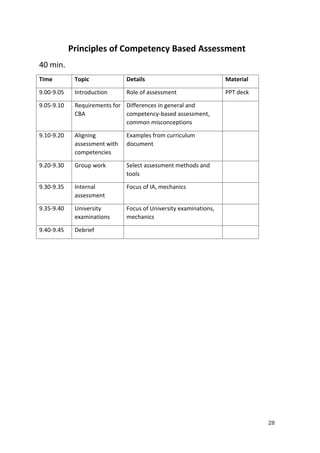
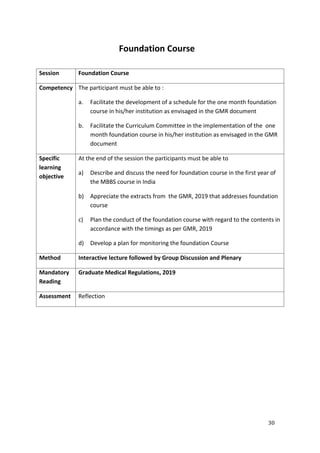
Total Time : 45 mins
Time Agenda/Activity Materials
15
mins
Introduction to Foundation course
Scope and need
PPT
10 min Discussion in small groups on
a. Challenges and suggestions
b. Session planning with regard to contents, faculty
c. Time table.
1. Orientation to medical profession & college [w.r.t GMR
9.1.2(a)]
2. Professional Development & Ethics [w.r.t AETCOM module]
3. Language & Computer skills [w.r.t GMR 9.1.2(b)]
4. Basic Skills Training [w.r.t GMR 9.1.2(c)]
20 min Plenary on the above (3 min presentation and 2 minutes discussion
from each group)](https://image.slidesharecdn.com/mci-cisp-240125043537-362576ba/85/MCI-CISP-pdf-31-320.jpg)