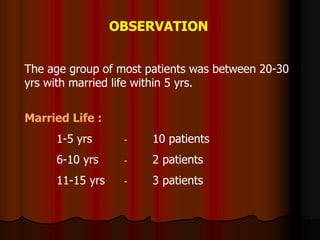
This document summarizes a study of 15 maternal deaths from gestational hypertension (PIH) at a tertiary hospital in India over 2 years. Most deaths were young, low-income, unbooked patients presenting near-term or postpartum with severe preeclampsia and multi-organ failure. Despite aggressive treatment with antihypertensives, diuretics, anticonvulsants and delivery, 11 patients died within 24 hours of admission in multi-organ failure, while 4 survived over 24 hours. The study concludes more needs to be done to provide proper antenatal care to rural populations, as all deceased patients were unbooked, and that critical care units are needed to better manage multi-organ