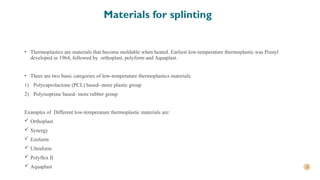
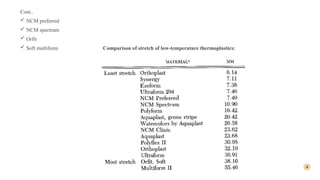
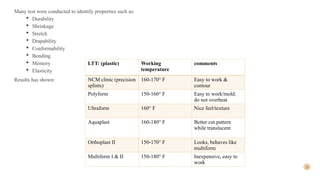
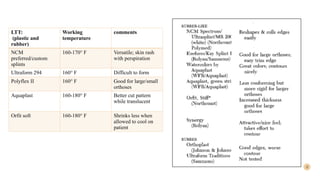
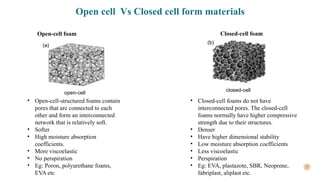
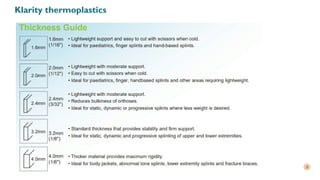
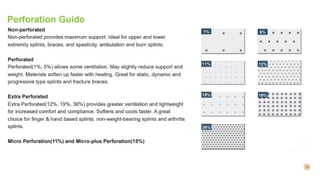
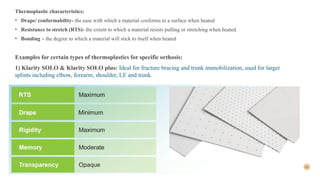
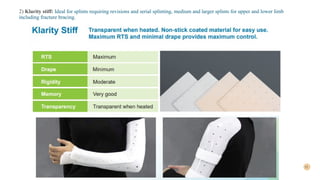
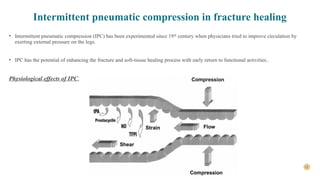
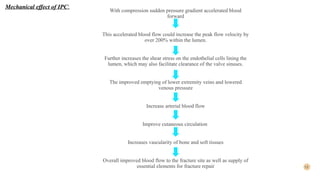
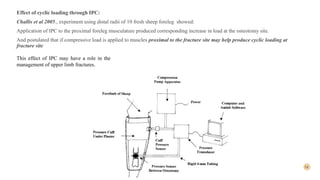
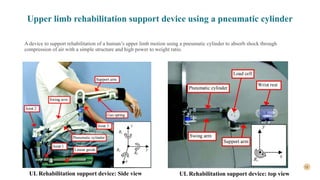
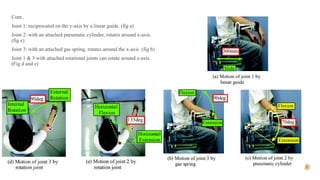
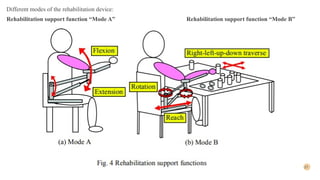
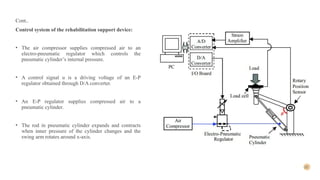
The document discusses materials for upper extremity fracture splints, including types of low-temperature thermoplastics and their properties, as well as intermittent pneumatic compression (IPC) and pneumatic actuators for rehabilitation. IPC enhances healing by improving blood flow and muscle strength recovery, while pneumatic actuators provide support for upper limb rehabilitation. Key aspects include the characteristics of thermoplastics used in splints and the design of rehabilitation devices employing pneumatic cylinders.