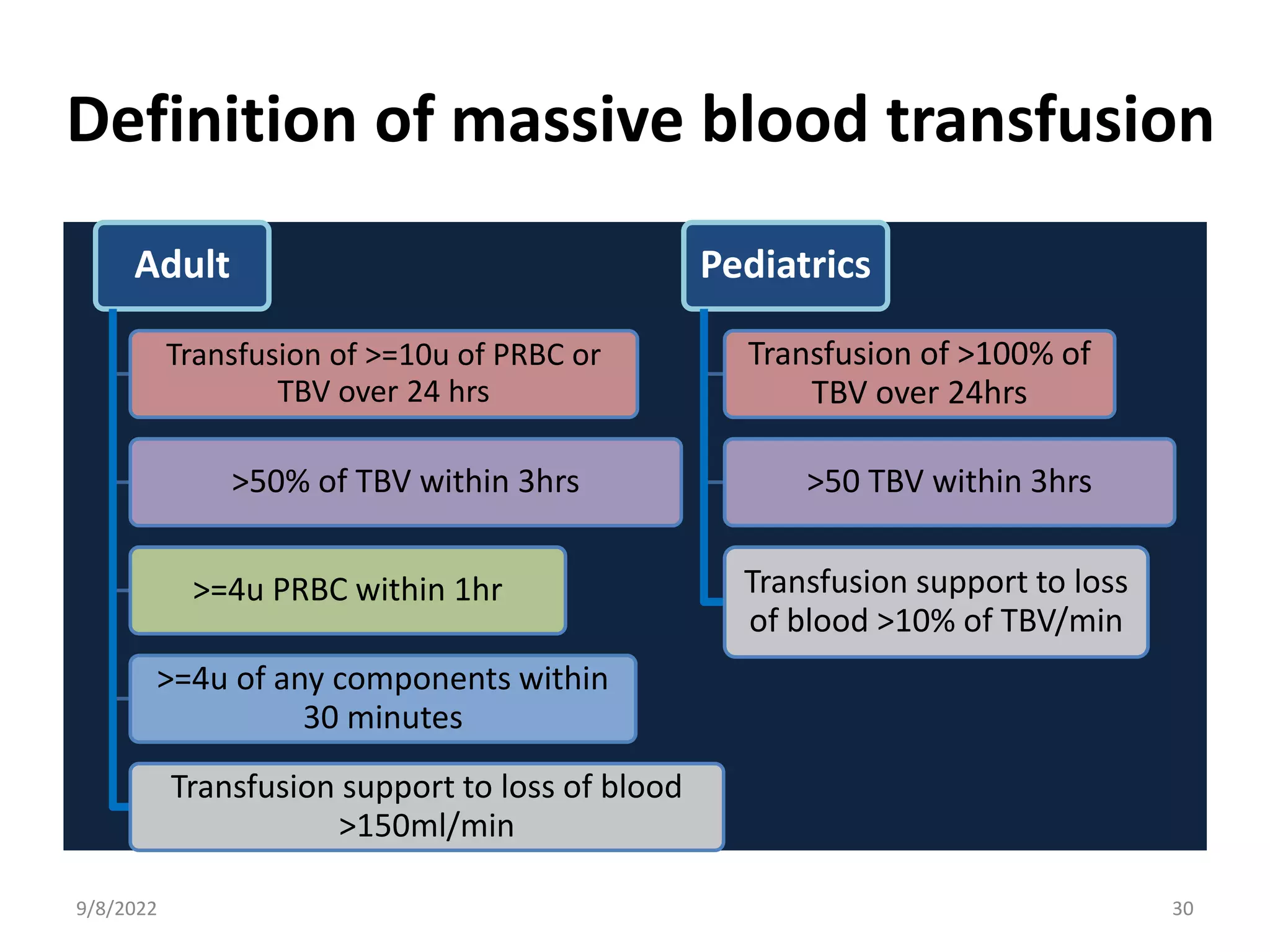
This document outlines the pathophysiology of blood loss and massive transfusion. It discusses hemostasis, the body's response to blood loss, trauma-induced coagulopathy, assessment of blood loss, hemostatic monitoring including viscoelastic tests, definitions of massive transfusion, indications and management including massive transfusion protocols, component ratios, and targets. It also covers special considerations for pediatric, obstetric, and liver disease populations.