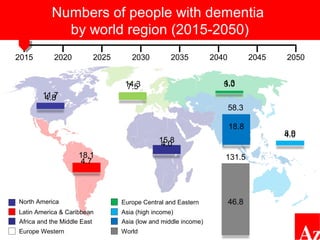
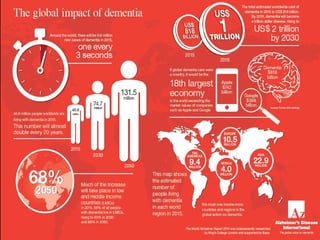
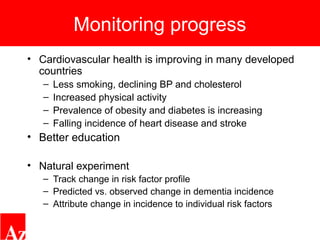
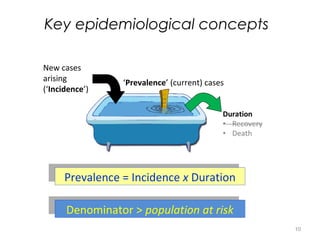
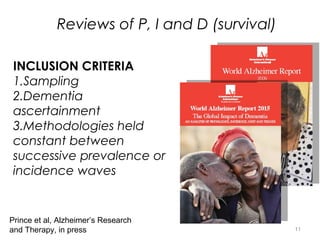
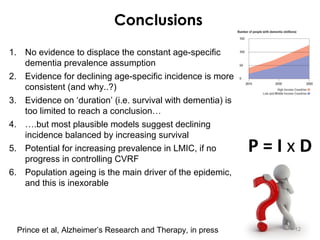
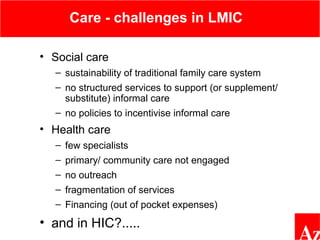
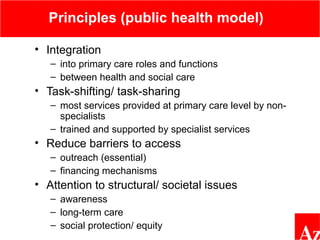
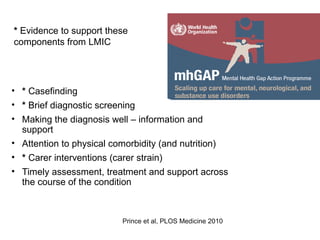
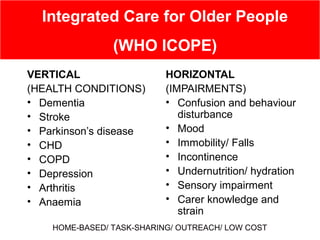
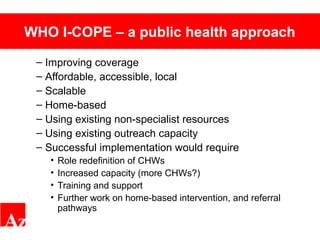
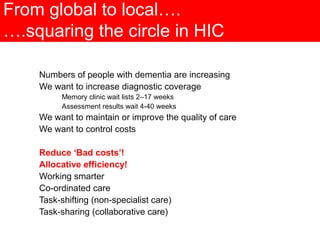
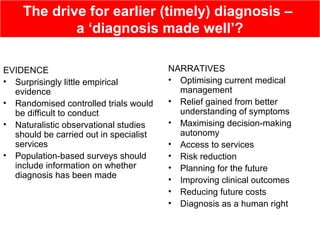
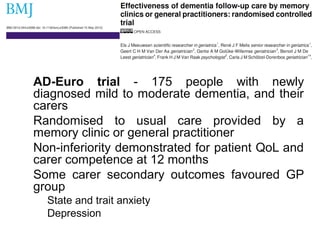
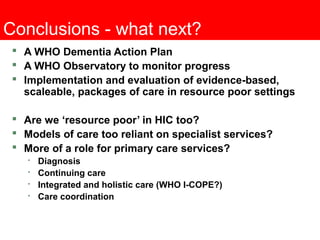
This document discusses global efforts to address dementia and presents strategies for improving dementia care. It notes that most of the burden of dementia is in low and middle income countries and outlines a public health approach. This includes integrating dementia care into primary care, task-shifting to train non-specialists, and addressing barriers to access. It also reviews evidence for approaches like the WHO ICOPE model and discusses challenges in high-income countries like increasing diagnostic rates and controlling costs while maintaining quality. Overall it advocates for implementing evidence-based packages of dementia care globally using scalable, affordable, home-based models.