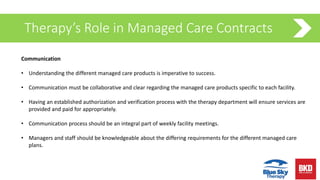
The webinar discusses managed care and the Patient-Driven Payment Model (PDPM), highlighting the importance of communication, collaboration, and understanding varied managed care products to optimize patient outcomes. It covers strategies for successful discharge planning, interdisciplinary coordination, and managing financial aspects within Medicare managed care. Additionally, it emphasizes the need for regular assessments and adjustments to ensure quality care and appropriate reimbursement.