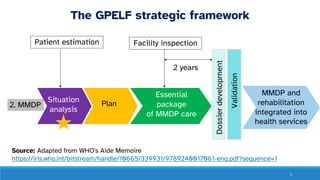
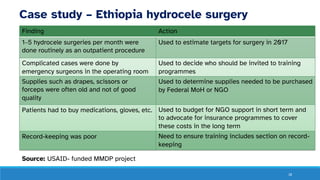
This module outlines the components and significance of conducting a situation analysis for lymphatic filariasis morbidity management and disability prevention (LF MMDP) program planning. It details methods for patient estimation, facility readiness, and the integration of MMDP into health services, as well as goals for future implementation. Case studies demonstrate the process of assessing and addressing the needs of patients and health facilities in various countries.