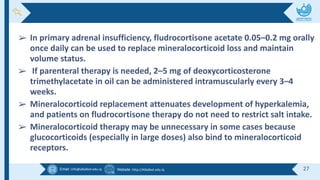
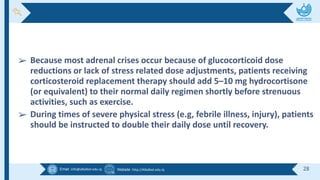
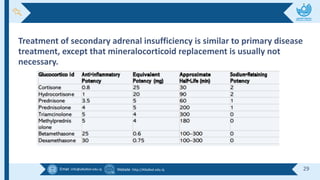
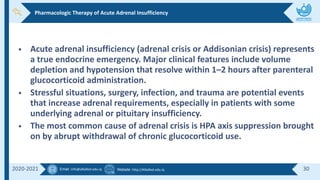
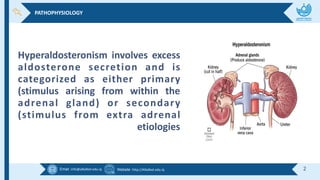
The document discusses adrenal gland disorders, focusing on hyperaldosteronism and adrenal insufficiency. It covers their causes, symptoms, diagnosis, and treatment options, highlighting the importance of screening and managing these conditions effectively. Key treatment strategies for hyperaldosteronism include surgical intervention and pharmacologic therapies, while adrenal insufficiency is managed with corticosteroids and patient education regarding stress management.
![Email :info@alkafeel.edu.iq Website :http://Alkafeel.edu.iq 21
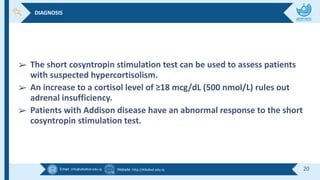
➢ Plasma ACTH levels are usually elevated (400– 2000 pg/mL or 88–440
pmol/L) in primary insufficiency versus normal to low (5–50 pg/mL or
1.1–11 pmol/L]) in secondary insufficiency.
➢ A normal cosyntropin stimulation test does not rule out secondary
adrenal insufficiency. Other tests include the insulin hypoglycemia test,
the metyrapone test, and the CRH stimulation test.](https://image.slidesharecdn.com/lecture2therapeuticsii-1-241214104741-0d1b6b2b/85/lecture-2-therapeutics-II-1-pdf-21-320.jpg)