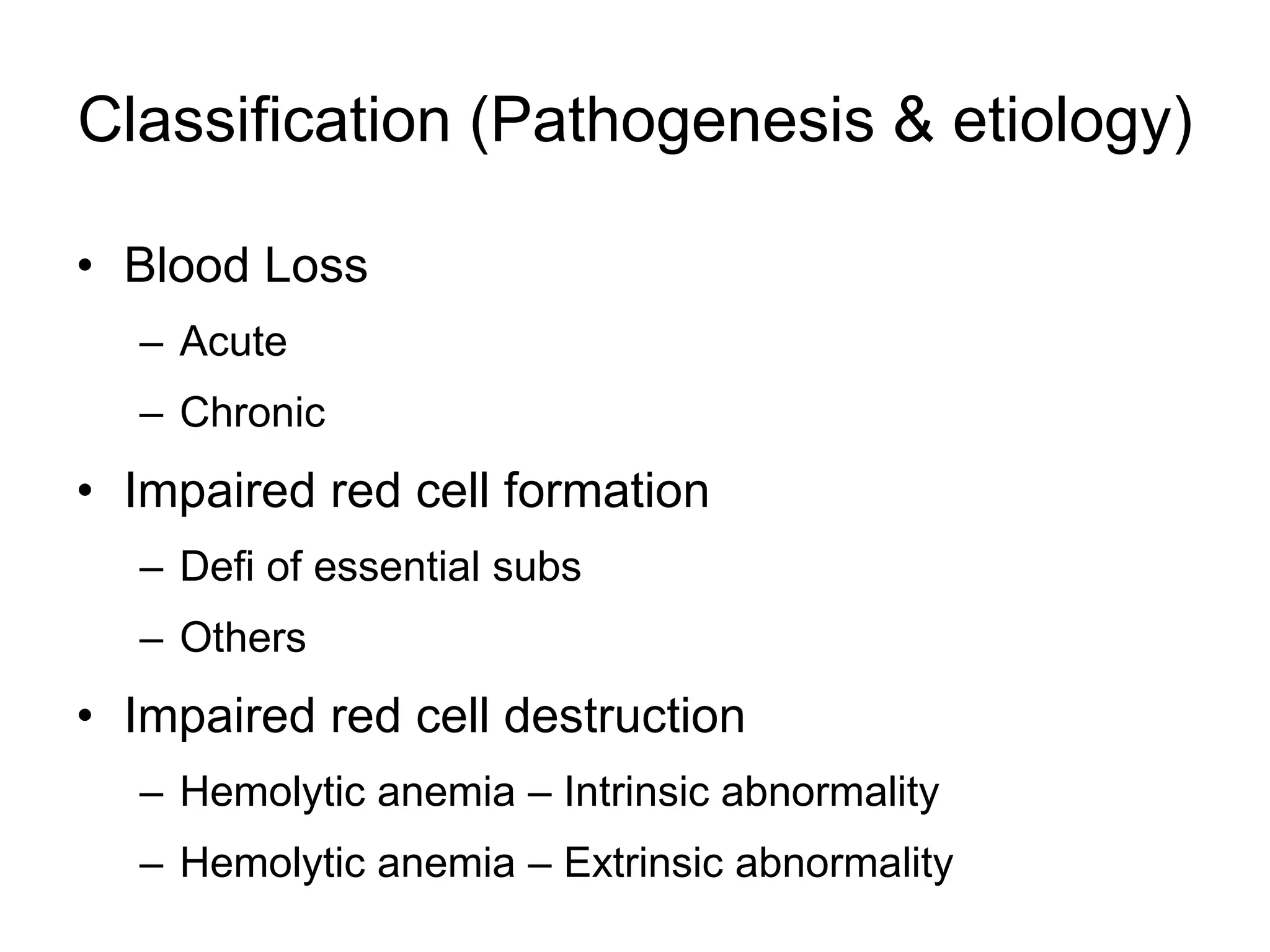
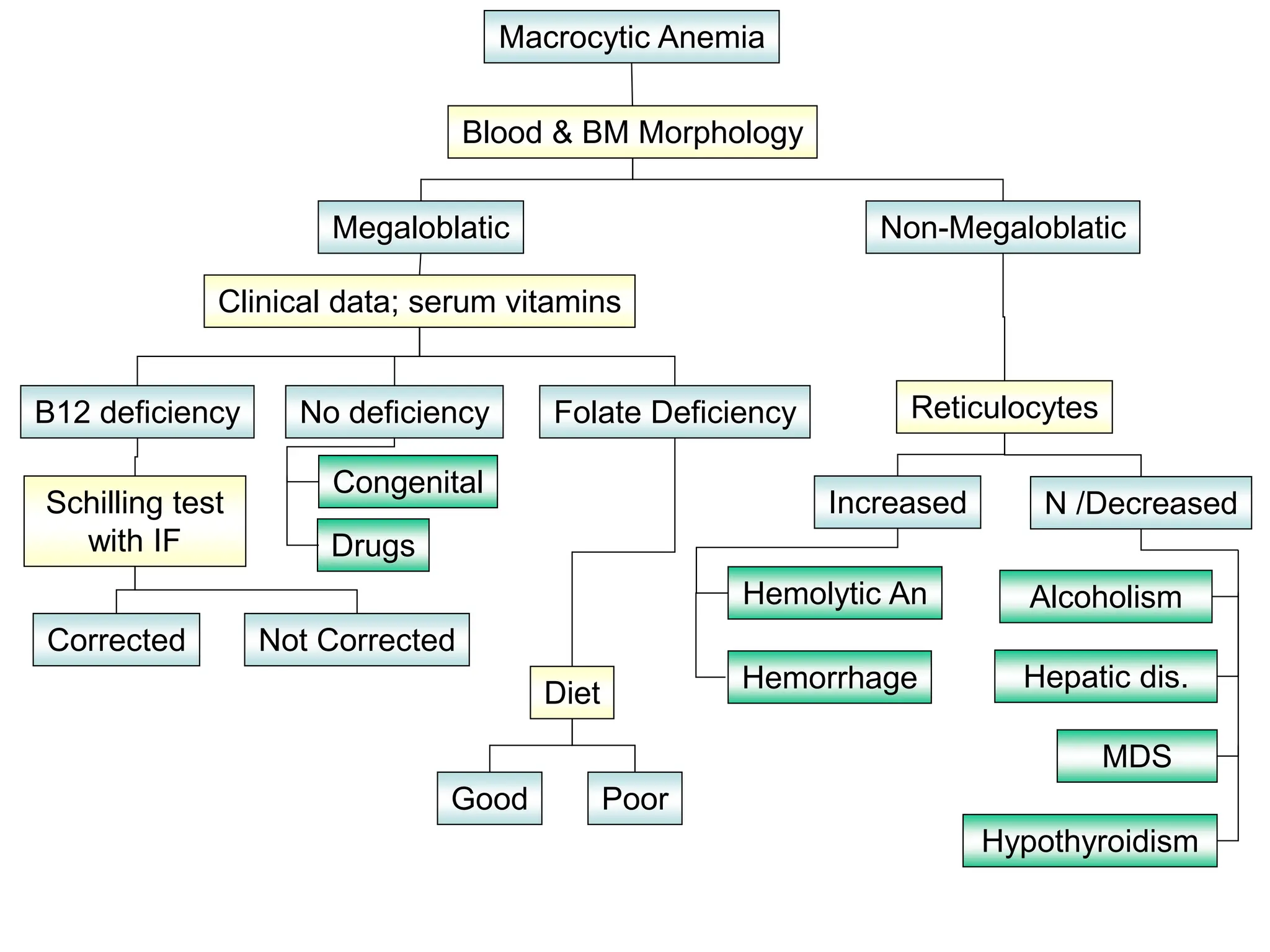
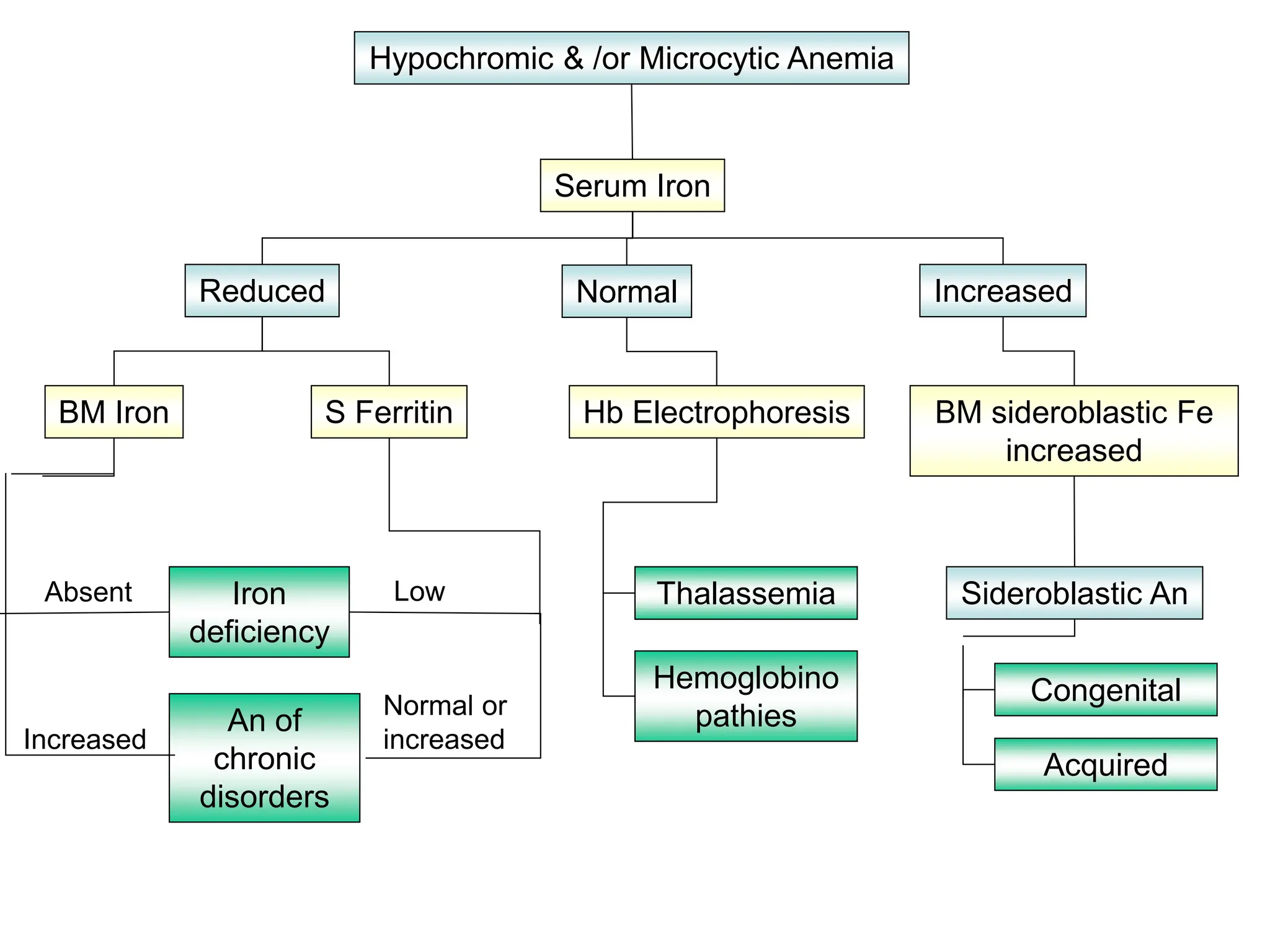
This document provides an overview of approaches to classifying and diagnosing anemia. It defines anemia and outlines important factors to consider, such as looking for the primary cause. Anemia is classified based on pathogenesis and etiology into categories like blood loss, impaired red cell formation, and impaired red cell destruction. Mean corpuscular volume (MCV) is used to classify chronic anemias as microcytic, normocytic, or macrocytic. Differential diagnoses are considered based on additional laboratory findings and clinical presentation for each type. General evidence of hemolysis is also outlined.