J Wound Ostomy Continence Nurs. 2015;42(2)151-154.Published.docx
- 1. J Wound Ostomy Continence Nurs. 2015;42(2):151-154. Published by Lippincott Williams & Wilkins WOUND CARE Copyright © 2015 by the Wound, Ostomy and Continence Nurses Society™ J WOCN ■ March/April 2015 151 Patient safety and prevention of harm are foundational principles of healthcare, and nursing in particular, yet pa- tients continue to develop pressure ulcers while under our care. Hospital-acquired pressure ulcers (HAPUs) cause pain, loss of function, and infection, extend hospital stays, and increase costs. The cost of treating these wounds is approx- imately $11 billion a year. In spite of progress in wound care products, support surfaces, and prevention methods, occurrences of pressure ulcers persist. 1 Medical device-re- lated HAPUs are common in both adults and children in the acute care setting. Medical Device–Related Hospital- Acquired Pressure Ulcers Development of an Evidence-Based Position Statement Joyce Pittman � Terrie Beeson � Jessica Kitterman � Shelley Lancaster � Anita Shelly ■ ABSTRACT Hospital-acquired pressure ulcers (HAPUs) are a problem in the acute care setting causing pain, loss of function, infection, extended hospital stay, and increased costs. In
- 2. spite of best practice strategies, occurrences of pressure ulcers continue. Many of these HAPUs are related to a medical device. Correct assessment and reporting of device-related HAPUs were identifi ed as an important issue in our organization. Following the Iowa Model for Evidence-Based Practice to Promote Quality Care, a task force was created, a thorough review of current evidence and clinical practice recommendations was performed, and a defi nition for medical device-related HAPU and an evidence-based position statement were developed. Content of the statement was reviewed by experts and appropriate revisions were made. This posi- tion statement provides guidance and structure to accu- rately identify and report device-related HAPU across our 18 healthcare facilities. Through the intentional focus on pressure ulcer prevention and evidence-based practice in our organization and the use of this position statement, identifi cation and reporting of device-related HAPUs have improved with a decrease in overall HAPU rates of 33% from 2011 and 2012. This article describes the development and implementation of this device-related HAPU position statement within our organization. KEY WORDS: Evidence-based , Iowa Model , Medical device- related pressure ulcers , Position statement A pressure ulcer can occur wherever external pressure impairs circulation to the skin. Pressure ulcers have been defi ned by the National Pressure Ulcer Advisory Panel (NPUAP) as “a localized injury to the skin and/or underly- ing tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear.” 2 (p6) This defi nition is helpful but many pressure ulcers occur as a result of external pressure from medical devices that do not completely fi t this defi nition. The NPUAP addressed device- related HAPUs, which develop on mucosal membranes by
- 3. issuing a statement describing the inappropriate use of stag- ing/category classifi cation due to anatomical differences between mucosal membrane with skin structures. The National Database of Nursing Quality Indicators recom- mends using the term “indeterminate” when classifying HAPUs over mucosal membranes when reporting HAPU. 3 , 4 However, neither of these recommendations provides a clear and concise defi nition for all device-related HAPUs. Hospital-acquired pressure ulcer development is con- sidered a quality indicator across healthcare systems. 5 Healthcare facilities are required to track and report HAPU rates. In our large academic healthcare system, prevention and accurate identifi cation and classifi cation of HAPUs are a high priority. Monthly skin audits within our facility found that a high percentage, often more than 50%, of HAPUs are device related. In addition, the identifi cation, � Joyce Pittman, PhD, ANP-BC, FNP-BC, CWOCN, Indiana University Health–Methodist, Indiana University School of Nursing, Indianapolis. � Terrie Beeson, MSN, RN, CCRN, ACNS-BC , Indiana University Health- University Hospital, Indianapolis. � Jessica Kitterman, BSN, CWOCN , Indiana University Health- Ball Hospital, Muncie. � Shelley Lancaster, MSN, CNS, CWOCN , Indiana University Health- West Hospital, Indianapolis. � Anita Shelly, MSN, CNS, CWOCN , Indiana University Health- Riley Hospital, Indianapolis. The authors declare no confl icts of interest. Correspondence: Joyce Pittman, PhD, ANP-BC, FNP-BC,
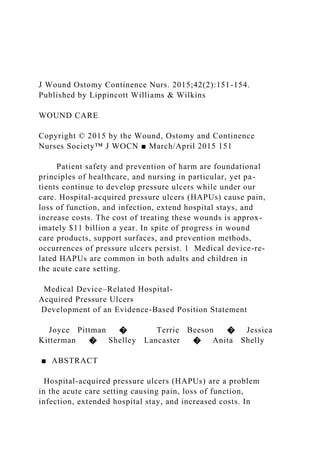
- 4. CWOCN, Indiana University Health–Methodist, Indiana University School of Nursing, 1701 Senate Blvd, Room B651, Indianapolis, IN 46202 ( [email protected] ). DOI: 10.1097/WON.0000000000000113 Copyright © 2015 Wound, Ostomy and Continence Nurses Society™. Unauthorized reproduction of this article is prohibited. JWOCN-D-14-00006_LR 151JWOCN-D-14-00006_LR 151 21/02/15 2:01 PM21/02/15 2:01 PM 152 Pittman et al J WOCN ■ March/April 2015 defi nition, and reporting of these types of HAPU are in- consistent with high variation across this organization’s acute care facilities. Therefore, a task force was created and given the directive to explore this issue. The purpose of this article is to describe the process this task force used to address this important issue. ■ Development of the Project When examining a practice issue or problem, it is helpful to use a model that provides a guide to identify areas of clinical inquiry through synthesis and application of research fi nd- ings. 6 One such model is the Iowa Model of Evidence-based Practice to Promote Quality Care (Figure 1). It provides guid- ance for nurses to use research fi ndings for improvement of patient care. Using this model, we fi rst created a task force that included members of our Pressure Ulcer Prevention sys-
- 5. temwide committee. Task force members represented 4 of our adult acute care facilities and our childrens’ hospital. Four of the task force members were certifi ed WOC nurses, 3 were also masters prepared and/or a clinical nurse special- ist, and 1 member was doctorally prepared. Using the Iowa Model of Evidence-based Practice to Promote Quality Care, the task force identifi ed medical device-related pressure ul- cers as a problem-focused trigger, a clinical problem, and a priority of the healthcare organization. This was an impor- tant fi rst step because a topic that is aligned with the strate- gic goals of the organization and embraced by staff has a high likelihood of being adopted by those providing care. 6 In addition, connecting the knowledge gained from research to an organizational initiative that has relevance to both the organization and the WOC nurse creates an opportunity and environment for support that might not be available if the topic were chosen to fulfi ll local interests alone. 7 Developing a well-formulated purpose statement is benefi cial once the topic or problem is identifi ed. The purpose statement directs the evidence search, helps focus reading, and defi nes the boundaries and limits around the work to be accomplished. Finally, we advocate formulat- ing a clear and concise purpose statement to assist with developing an appropriate implementation and evalua- tion plan. The task force was charged with developing a standardized, evidence-based defi nition for device-related HAPU, which would support appropriate identifi cation and reporting of these pressure ulcers. The next step in the Iowa Model is to appraise the evi- dence related to the question or purpose statement. In order to fi nd the most current new knowledge related to device-related pressure ulcers, a search was conducted of the current relevant literature. We searched the MEDLINE electronic database. Key search strategies were: (1) time
- 6. frame: 1996 to September 2012; (2) exp *“Equipment and Supplies”/ (312834); (3) exp *Pressure Ulcer/ep, et [Epidemiology, Etiology] (851); (4) 1 and 2 (84); (5) limit 3 to (English language and humans) (78); and (6) from 4 keep 2–4, 6, 13, 16–17, 20, 23–24, 26–31, 35–39, 53–54, 64, 69–71, 76–78 (30). This search identifi ed 30 references, which were reviewed by our team. The task force identifi ed the defi nition of medical de- vices by the Food Drug & Cosmetic Act as integral to de- veloping a defi nition of device-related HAPUs. The US Food and Drug Administration defi nes a medical device as “…an instrument, apparatus, implement, machine, con- trivance, implant, in vitro reagent, or other similar or re- lated article, including a component part, or accessory which is: recognized in the offi cial National Formulary, or the United States Pharmacopoeia, or any supplement to them, intended for use in the diagnosis of disease or other conditions, or in the cure, mitigation, treatment, or pre- vention of disease, in man or other animals, or intended to affect the structure or any function of the body of man or other animals, and which does not achieve any of its primary intended purposes through chemical action within or on the body of man or other animals and which is not dependent upon being metabolized for the achieve- ment of any of its primary intended purposes.” 8 (p1) Another important piece of evidence was that of the NPUAP and its work surrounding pressure ulcers. The NPUAP hosted a consensus conference in 2010 and again in 2014 to discuss the complexities of avoidable versus un- avoidable HAPUs. As a result of this work, NPUAP has led efforts of the wound and pressure ulcer expert community in identifying key components related to pressure ulcer de- velopment and the complexities surrounding these wounds.
- 7. This work is in its initial stages, but a state of the science article was published recently describing unavoidable pres- sure ulcer incidence and the key risk factors that infl uence them. 9 One of these key risk factors identifi ed is that of med- ical devices. Medical device-related pressure ulcers are diffi - cult to prevent as they are necessary for treatment. They are also challenging to assess due to the inability to remove them in certain instances, and they may produce compro- mise of underlying tissue due to moisture or edema. Many states are recognizing the importance of HAPUs and are requiring the reporting of prevalence of HAPUs as a quality measure. Minnesota used data collected through mandatory statewide adverse health events reporting sys- tem to identify trends in causative factors for device-re- lated pressure ulcers. An interdisciplinary team convened to develop best practices for prevention of pressure ulcers related to the use of medical devices. 10 Although the fi nd- ings from this report are helpful, no defi nitive defi nition for device-related HAPUs was described. ■ Implementation of the Project Using the US Food and Drug Administration defi nition for medical devices, evidence-based guidelines, and position statements from various organizations, and results of an ex- pert review, the task force defi ned device-related skin injury to those devices that were medical and external. The task force identifi ed 2 critical elements to be included in the Copyright © 2015 Wound, Ostomy and Continence Nurses Society™. Unauthorized reproduction of this article is prohibited. JWOCN-D-14-00006_LR 152JWOCN-D-14-00006_LR 152 21/02/15 2:01 PM21/02/15 2:01 PM
- 8. J WOCN ■ Volume 42/Number 2 Pittman et al 153 Assemble Relevant Research & Related Literature Critique & Synthesize Research for Use in Practice NoYes Yes Is Change Appropriate for Adoption in Practice? Yes Institute the Change in Practice No Continue to Evaluate Quality of Care and New Knowledge No Disseminate Results Problem Focused Triggers 1. Risk Management Data 2. Process Improvement Data 3. Internal/External Benchmarking Data
- 9. 4. Financial Data 5. Identification of Clinical Problem Knowledge Focused Triggers 2. National Agencies or Organizational Standards & Guidelines 3. Philosophies of Care 4. Questions from Institutional Standards Committee 1. New Research or Other Literature Consider Other Triggers Is this Topic a Priority For the Organization? Form a Team Is There a Sufficient Research Base? Pilot the Change in Practice 1. Select Outcomes to be Achieved 2. Collect Baseline Data 3. Design Evidence-Based Practice (EBP) Guideline(s)
- 10. 4. Implement EBP on Pilot Units 5. Evaluate Process & Outcomes 6. Modify the Practice Guideline Base Practice on Other Types of Evidence: 1. Case Reports 2. Expert Opinion 3. Scientific Principles 4. Theory Conduct Research Monitor and Analyze Structure, Process, and Outcome Data • Environment • Staff • Cost • Patient and Family The Iowa Model of Evidence-Based Practice to Promote Quality Care DO NOT REPRODUCE WITHOUT PERMISSION Revised April 1998 © UIHC = a decision point Titler, M.G., Kleiber, C., Steelman, V.J., Rakel., B. A., Budreau, G., Everett, L.Q., Buckwalter, K.C., Tripp-Reimer, T., & Goode C. (2001). The Iowa Model Of Evidence- Based Practice to Promote Quality Care. Critical Care Nursing Clinics of North America, 13(4), 497-509. REQUESTS TO:
- 11. Department of Nursing University of Iowa Hospitals and Clinics Iowa City, IA 52242-1009 FIGURE 1. The Iowa Model of Evidence-Based Practice to Promote Quality Care. Reprinted with permission from the University of Iowa Hospitals and Clinics and Marita G. Titler, PhD, RN, FAAN, Copyright 1998. For permission to use or reproduce the model, please contact the University of Iowa Hospitals and Clinics at 319-384-9098 or [email protected] Copyright © 2015 Wound, Ostomy and Continence Nurses Society™. Unauthorized reproduction of this article is prohibited. JWOCN-D-14-00006_LR 153JWOCN-D-14-00006_LR 153 21/02/15 2:01 PM21/02/15 2:01 PM 154 Pittman et al J WOCN ■ March/April 2015 defi nition of device-related HAPUs: (1) NPUAP defi nition of pressure ulcers provides the basis of the defi nition and (2) device-related HAPUs will be limited to external medical de- vices. After a thorough review of the evidence and using clinical practice expertise, an evidence-based device-related HAPU defi nition for adults and pediatrics was developed. A device-related HAPU is defi ned as a localized injury to the skin and/or underlying tissue including mucous membranes, as a result of pressure, with a history of an external medical device at the location of the ulcer, and mirrors the shape of the device. This defi nition provides needed guidance, struc- ture, and process to assist with prevention, identifi cation,
- 12. reporting, and treatment of medical device-related HAPU. The task force used this evidence-based defi nition to de- velop the Medical Device-Related Pressure Ulcer Position Statement. Following the format example of the Wound, Ostomy and Continence Nursing Society and other organi- zations, a position statement was developed. In order to improve the content validity of the position statement, ex- perts in wound management and pressure ulcers were asked to review the content. Based on their recommendations, appropriate revisions were incorporated into the document. The next step in the Iowa Model is to move the evi- dence into practice. Effective dissemination of evidence includes mindful communication among opinion leaders, change champions, core groups of infl uence, and aca- demic detailing. Opinion leaders were defi ned as those col- leagues who are viewed as important and respected sources of infl uence among their peers. Change champions embrace and demonstrate the persistence necessary to pro- mote the adoption of evidence. The task force disseminated the position statement by informing various systemwide leadership groups involved in patient quality/safety, systemwide pressure ulcer pre- vention committee, facility-specifi c WOC nurse experts, and facility-specifi c direct-care nurse wound teams. Dissemination continues as the use of the Medical Device- Related Pressure Ulcer Position Statement is integrated into the process of conducting our monthly facility-wide pressure ulcer prevalence surveys. ■ Conclusion A pressure ulcer may occur wherever external pressure im- pairs circulation to the skin. Pressure ulcers cause pain, loss
- 13. of function, and infection, extend hospital stays, and in- crease cost. In addition, pressure ulcer development is con- sidered a quality indicator across healthcare systems. 5 Increased scrutiny and reduced payment or nonpayment for HAPU by the Centers for Medicare & Medicaid Services has made the prevention and early detection of pressure ulcers a prominent quality improvement initiative of healthcare systems across the country. A key component in prevention and detection of pressure-related injury is an accurate skin assessment. In order to perform an accurate skin assessment, an evidence-based defi nition for device- related pressure ulcers is crucial. Our Device-Related Pressure Ulcer Position Statement guides practice, educa- tion, and research within this healthcare organization. This defi nition is used when identifying, reporting, treating, and developing prevention strategies for device-related HAPU. It has proven useful for distinguishing between pressure ulcers resulting from an external medical device versus nonmedical device. Through the intentional focus on pres- sure ulcer prevention and evidence-based practice in our organization and the use of this position statement, identi- fi cation and reporting of medical device-related HAPUs have improved with a decrease in overall HAPU rates of 33% from 2011 and 2012. This concise and evidence-based position statement supports appropriate and consistent identifi cation and reporting of medical device–related pres- sure ulcers. Staging of these ulcers continues to follow the staging recommendations of NPUAP and National Database for Nursing Quality Indicators reporting instructions. ■ References 1. Ayello E , Lyder C . Protecting patients from harm: preventing pressure ulcers . Nursing 2007 ; 37 : 36-40 .
- 14. 2. EPUAP/NPUAP . European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Treatment of Pressure Ulcers: Quick Reference Guide . Washington, DC : National Pressure Ulcer Advisory Panel ; 2009 . 3. Berquist-Beringer S , Davidson J . NDNQI: Pressure Ulcer Training . 2013 . Accessed December 18, 2014 . at https://members.nursing quality.org/NDNQIPressureUlcerTraining/ 4. NPUAP. Mucosal Pressure Ulcers: An NPUAP Position Statement 2012. Accessed December 18, 2014 at http://www.npuap.org/ wp-content/uploads/2012/03/Mucosal_Pressure_Ulcer_ Position_Statement_fi nal.pdf 5. Centers for Medicare & Medicaid Services. Hospital- Acquired Conditions and Present on Admission Indicator Reporting Provision. Accessed December 18, 2014 at http://www.cms .gov/Outreach-and-Education/Medicare-Learning-Network- MLN/MLNProducts/Downloads/wPOAFactSheet.pdf 6. Titler M , Kleiber C , Steelman V , et al. The Iowa model of evidence-based practice to promote quality care . Crit Care Nurs Clin North Am. 2001 ; 13 ( 4 ): 497-509 . 7. Stanley T , Sitterding M , Broome M , McCaskey M . Engaging and developing research leaders in practice: Creating a foundation for a culture of clinical inquiry . J Pediatr Nurs. 2011 ; 26 :
- 15. 480-488 . 8. Food and Drug Administration . Is the product a medical de- vice ? http://www.fda.gov/MedicalDevices/DeviceRegulation andGuidance/Overview/ClassifyYourDevice/ucm051512.htm . Published 2013. Accessed December 16, 2013. 9. Edsberg LE , Langemo D , Baharestani MM , Posthauer ME , Goldberg M . Unavoidable pressure injury: state of the science and consensus outcomes . J Wound Ostomy Continence Nurs . 2014 ; 41 ( 4 ): 313-334 . 10. Apold J , Rydrych D . Preventing device- related pressure ulcers: using data to guide statewide change . J Nurs Care Qual . 2012 ; 27 ( 1 ): 28-34 . The CE test for this article is available online only at the journal website, jwocnonline.com, and the test must be taken online at NursingCenter.com/CE/JWOCN. Copyright © 2015 Wound, Ostomy and Continence Nurses Society™. Unauthorized reproduction of this article is prohibited. JWOCN-D-14-00006_LR 154JWOCN-D-14-00006_LR 154 21/02/15 2:01 PM21/02/15 2:01 PM Running head: NURSING RESEARCH UTILIZATION PROJECT PROPOSAL 1
- 16. NURSING RESEARCH UTILIZATION PROJECT PROPOSAL: 7 title page Methods for monitoring solution implementation using the Iowa Model The success of the solution implementation project relies heavily on the monitoring and evaluating of the project. The Iowa Model of Evidence Based Practice will be used to guide the project which relies on feedback loops which make the continued monitoring and evaluating of structures, processes, and outcome data a crucial part in its success. One of the first steps in the model requires that the practice question be aligned with the goals of the organization. This project has been requested of management and fits perfectly with the goal of improved patient care and improved outcomes. The continued monitoring of this alignment will be necessary with management and stakeholders and the ongoing results will be reviewed with them on an ongoing regular basis. The Iowa Model also stipulates the development and use of a team to gather, analyze, and critique the literature and its utilization in clinical practice. The team has already been assembled and includes member from various disciplines. This group will meet on a regular basis to refine the project and to move the project forward and to analyze and evaluate the results. A method to monitor deadlines and interim goals will be established and followed. Methods to Evaluate
- 17. During the pilot, staff compliance will be monitored to ensure the process is utilized correctly and that accurate data is being collected. Spot checks will be completed by at least two team members on a weekly basis and reported back to the committee. If the change works, it will become permanent and continued monitoring will be conducted to ensure workflow efficiency and continued SSI improvements. The overall success of the protocol will be measured by using the baseline measurement of SSIs from the entire OR suite within the last 12 months. After implementation, the team will collect SSI on a weekly basis from the entire OR suite and compare those results from that of the previous 12 month period. Outcome Measure Measurements are extremely important in quality management but in order to be effective, Smith (2014), insisted they be precise, useful, simple, and consistently reported. The outcome measure that will support the success of this project’s objective will be a reduction in SSI rates of at least three percent within 12 months of implementing the new protocol. This measure will be reported on a line graph (see Appendix for example) which will show a month-by-month comparison of SSI rates from the previous year. Line graphs are extremely useful when conducting an analysis of metrics as they provide practitioners a method to easily identify trends and improvement opportunities. Validity and Appropriateness The St. Mary’s Quality Improvement Department collects the data on SSI’s. This is the only data that is appropriate to ensure the outcome is achieved. The Quality Improvement Department has been doing this for many years as they do all infection rates within the facility. They will use the same method after the implementation of this protocol as they have for the past several years so the data and the process for collecting the data, has not changed and will not change for the duration of this project which increases the validity of this data. Resources and Methods Patient records are a useful data collection tool as they can
- 18. provide an overall view and details of a patient visit. St. Mary’s records are electronic and so any infections reported back from the lab will be flagged and sent directly to the OR manager and the Quality Improvement Department. This happens in real time and then monthly reports are automatically generated and distributed to the appropriate management team. In this case, reports will also be sent in real time to the new implementation team. No additional resources will be needed except for the time the team members need to meet. Feasibility The evaluation plan for the solution implementation is feasible and is actually being requested from OR management and surgeons. The problem was identified in 2013, yet it has yet to be addressed by the appropriate staff. The team has already been assembled and providing them with the details of an evidence-based solution along with an implementation and evaluation plan, makes this an easy potential solution. The Iowa Model of Evidence Based Practice will be used to guide the project which incorporates natural feedback loops as part of the process making the evaluation part of the normal everyday process. The evaluation plan requires very few resources with virtually no added cost to the departmental budget.
- 19. Appendix References SSI Rates 2014 vs 2015 2014 4.3 5.4 3.8 4.4000000000000004 3.8 5.3 6 5.4 4.4000000000000004 3.7 5.7 6.2 2015 2.4 2.2000000000000002 0 2.2999999999999998 1.9 2.5 2 1.3 0 2.1 1.1000000000000001 1.8 SSI Rate %