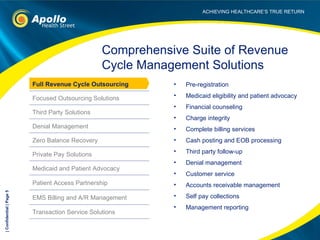
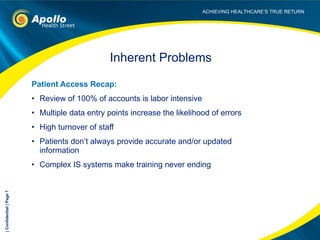
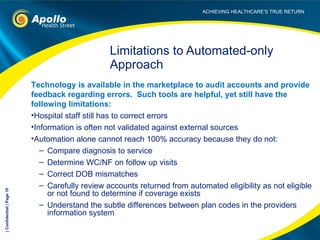
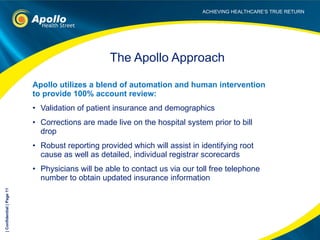
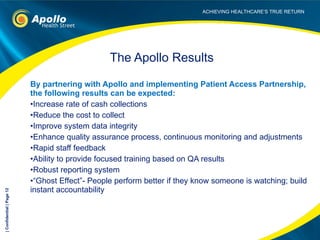
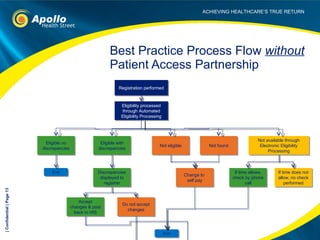
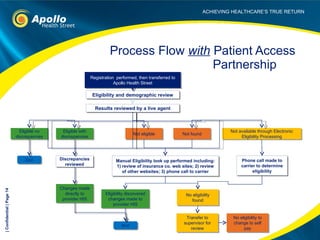
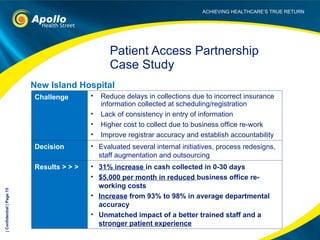
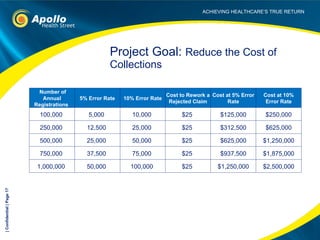
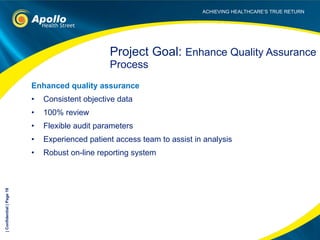
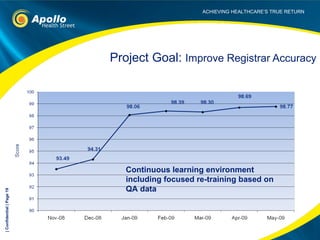
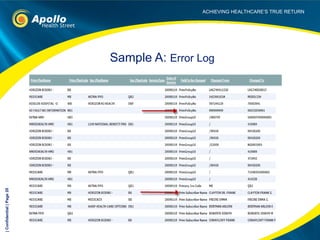
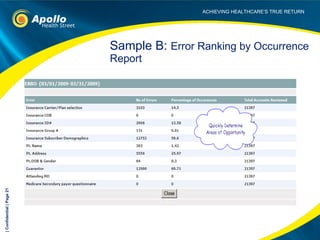
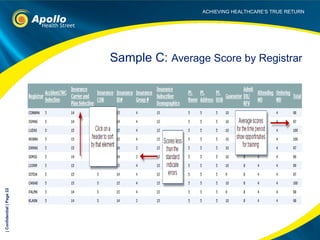
The document introduces Patient Access Partnership, a program from Apollo Health Street that audits and corrects 100% of patient accounts prior to billing to increase cash collections and decrease costs. It highlights the limitations of traditional and automated-only approaches to account review. The Partnership utilizes a blend of automation and human review to validate insurance and demographic information, make corrections directly in hospitals' systems, and provide robust reporting. The results hospitals can expect include increased cash collections, reduced costs to collect, improved data quality and a strengthened quality assurance process. It provides an example case study of a mid-sized hospital that saw a 31% increase in cash collected in 0-30 days and $5,000 monthly reduction in business office re-working






![Contact Information Michael S. Friedberg , FACHE, CHAM Associate Vice President, Patient Access Services [email_address] Office 973.233.7644 Mobile 732.809.0260 Learn more at www.apollohealthstreet.com](https://image.slidesharecdn.com/introducingpatientaccesspartnershipgeneric31810-12689459142724-phpapp01/85/Introducing-Patient-Access-Partnership-Generic-3-18-10-23-320.jpg)