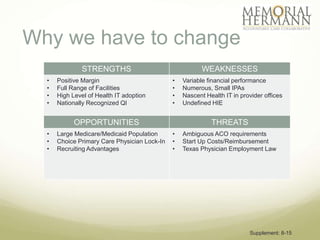
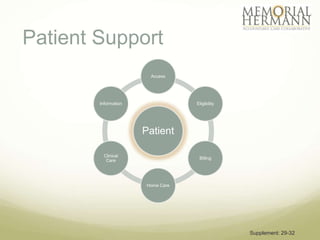
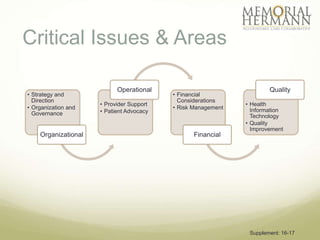
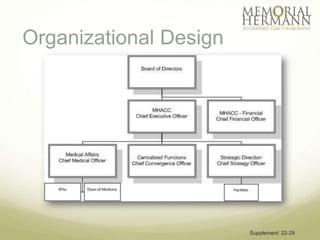
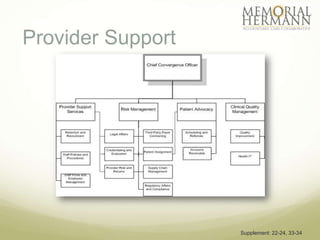
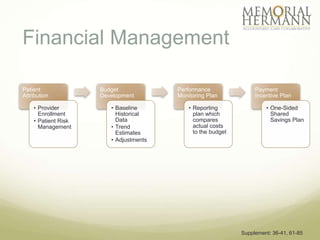
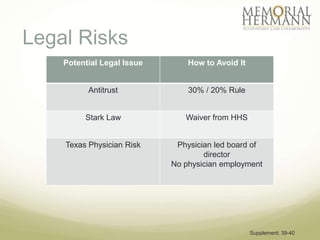
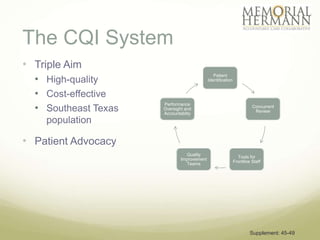
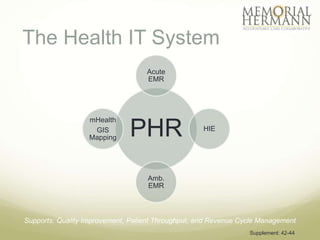
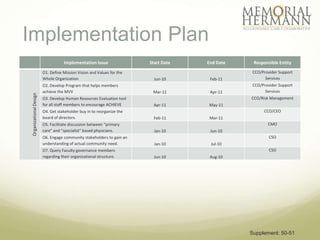
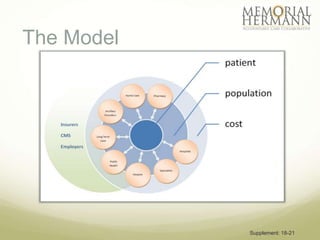
The document outlines a strategic plan for Memorial Hermann aimed at improving healthcare in Southeast Texas through a comprehensive approach that includes organizational design, provider support, and quality improvement. It highlights financial performance, operational challenges, and the need for stakeholder engagement, along with a detailed implementation plan with specific goals and timelines. The document emphasizes the importance of health IT, patient advocacy, and community needs in shaping future healthcare services.