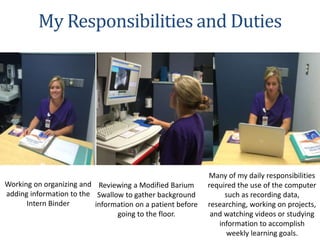
This document summarizes a health science internship completed at Grand Strand Regional Medical Center in the speech therapy department. The internship lasted from May to July 2016 and provided the intern with experience observing evaluations, treatments, and procedures. Through observing and assisting, the intern gained knowledge on common diagnoses and treatment approaches. The intern also completed various projects during the internship, including case studies, educational materials, and a study guide for future interns. The internship experience reinforced the intern's goal of becoming a speech language pathologist.