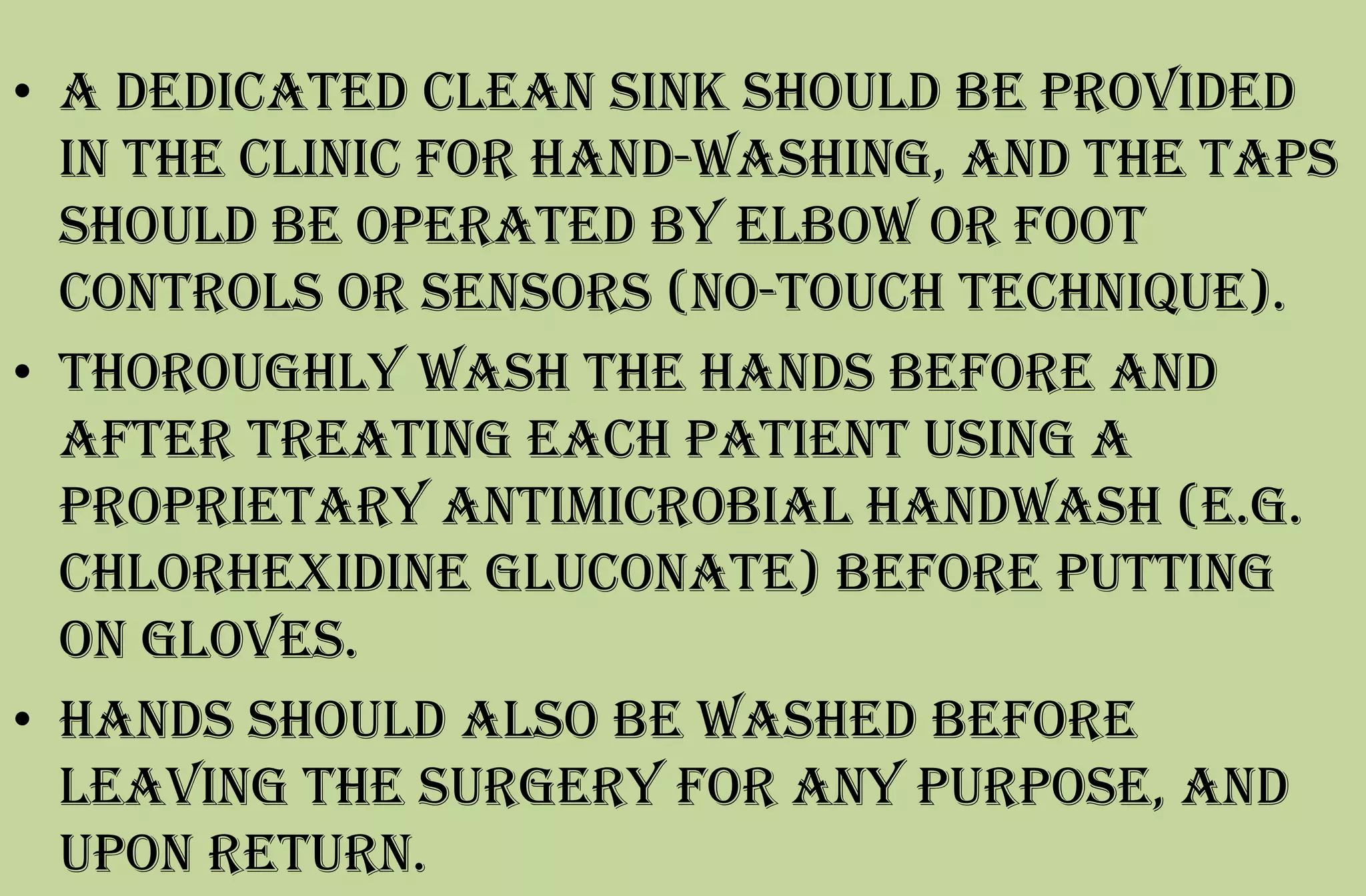
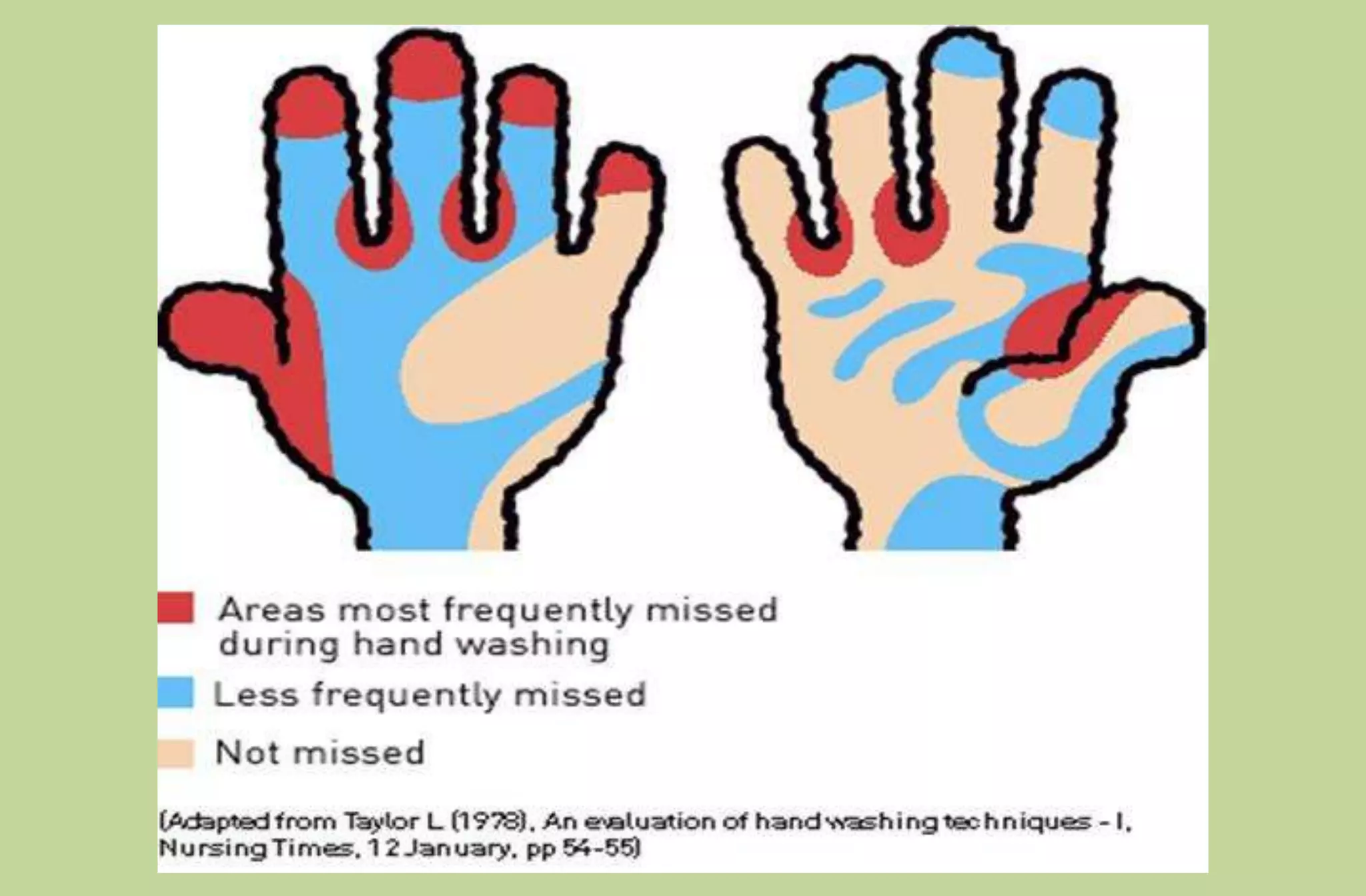
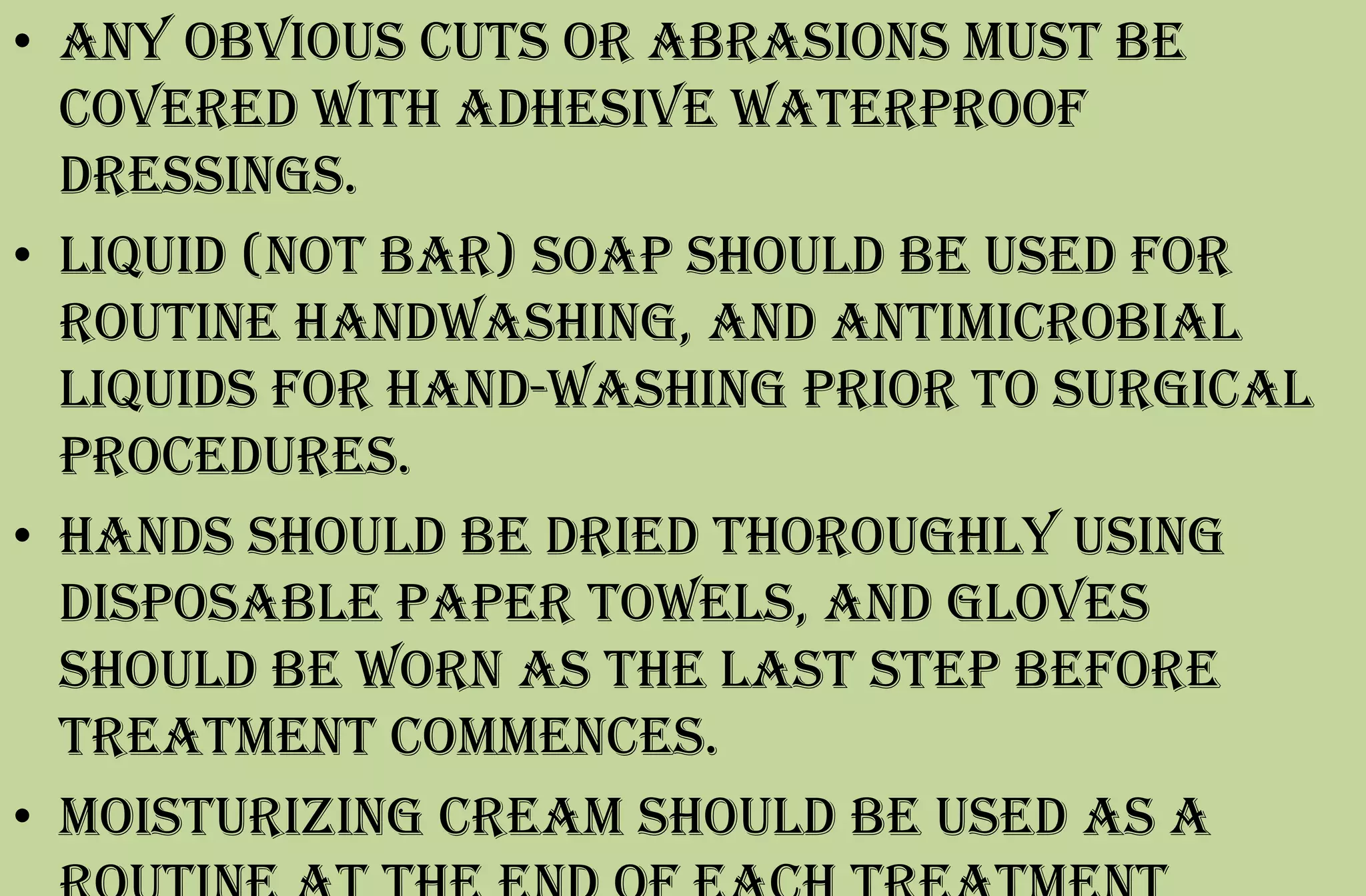
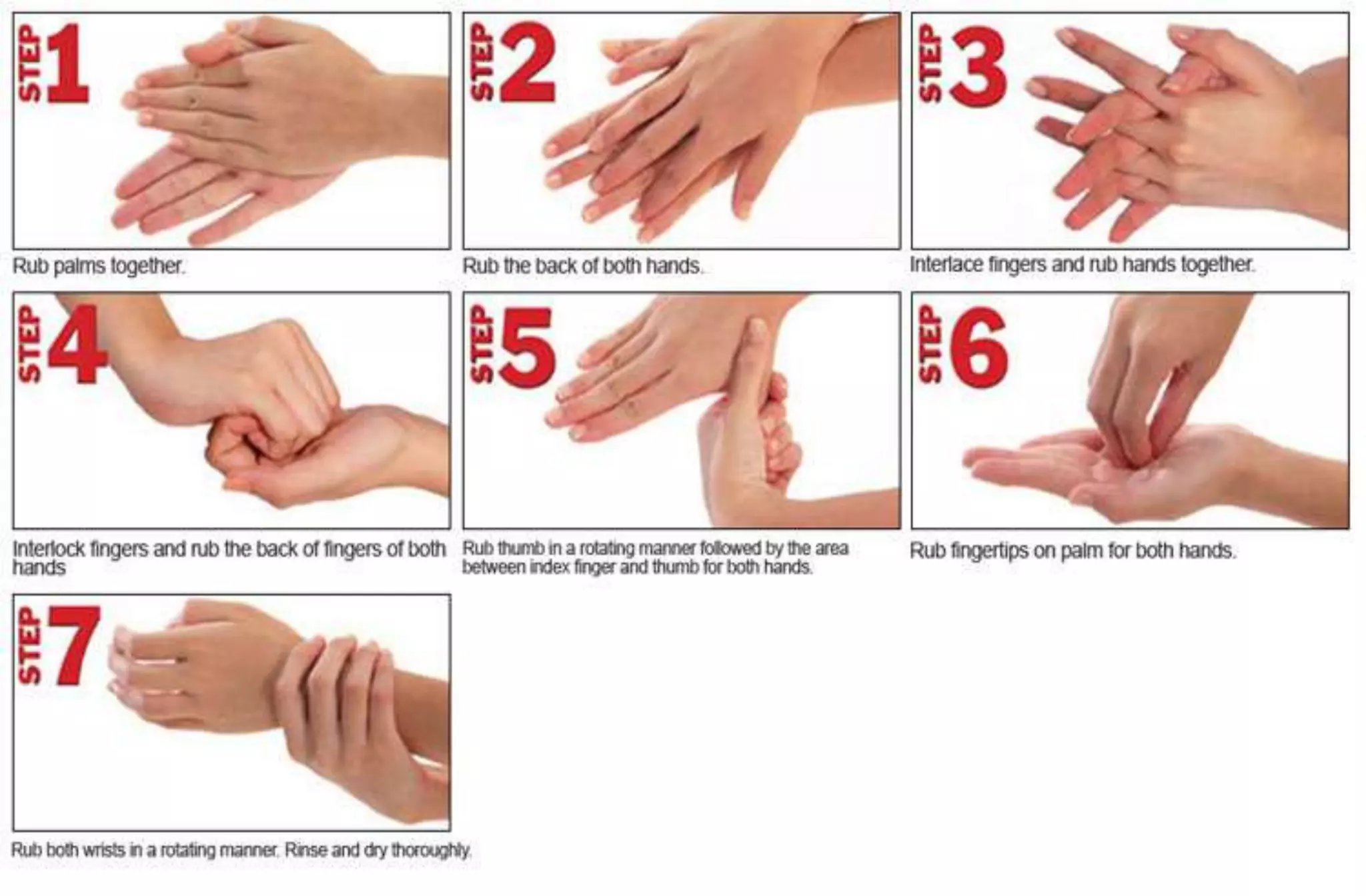
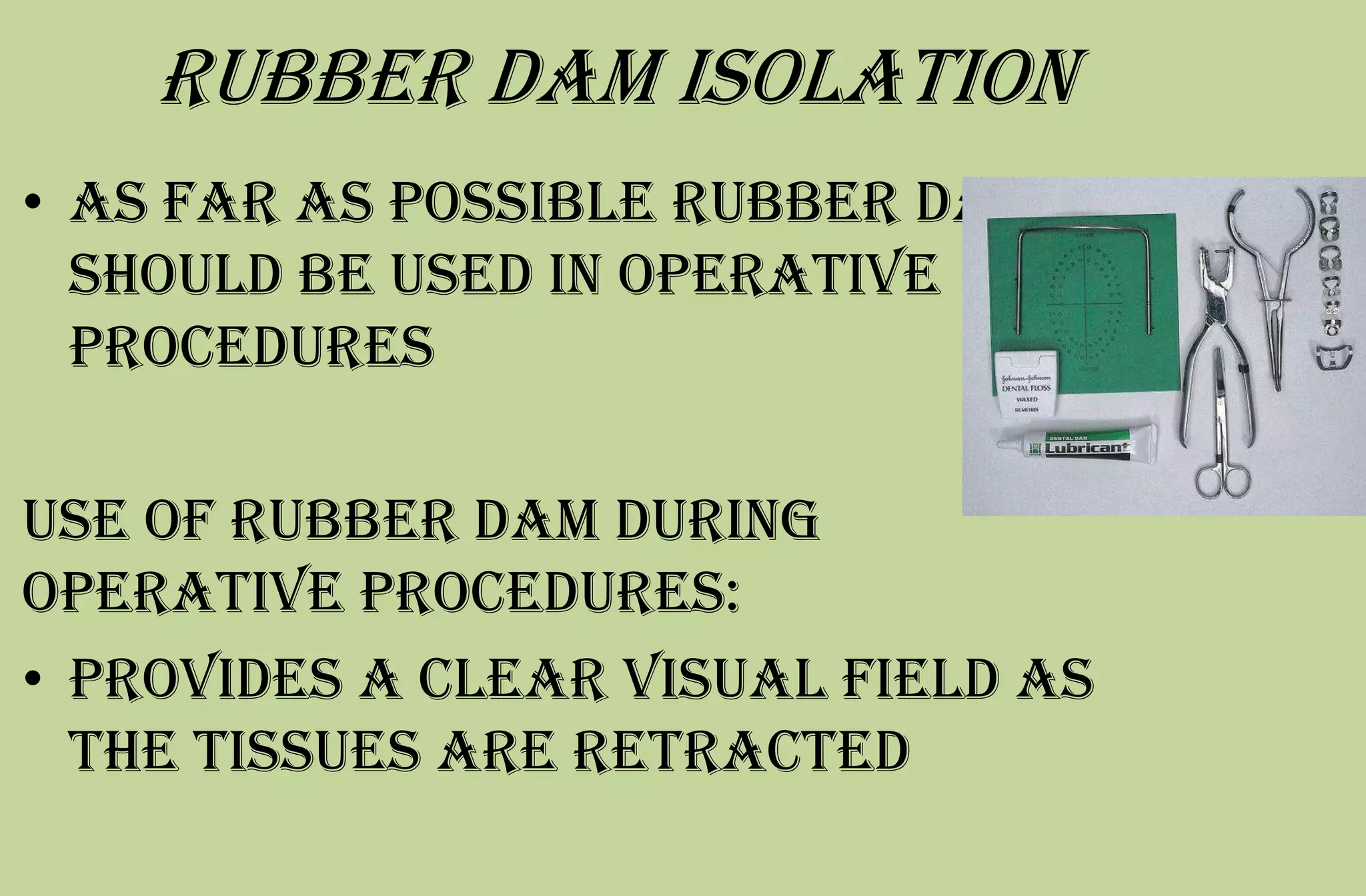
This document outlines infection control procedures for a dental office. It discusses evaluating patients for infectious diseases, using personal protective equipment like gloves and masks, sterilizing instruments, using disposable items, disinfecting surfaces, maintaining aseptic techniques in the lab, and proper disposal of waste. Proper hand hygiene and barrier protection when treating patients is emphasized. Sterile gloves and masks should be worn during treatment and high-speed procedures to prevent spread of aerosols. Instruments should be sterilized and stored properly. Rubber dams should be used when possible to provide a clear field and reduce aerosolization of fluids.