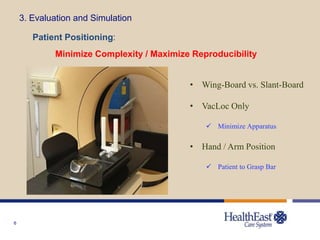
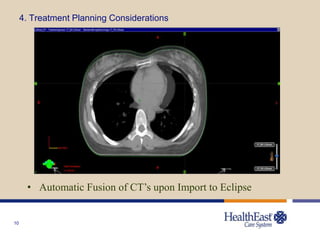
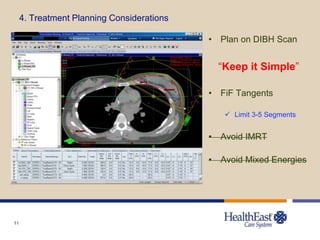
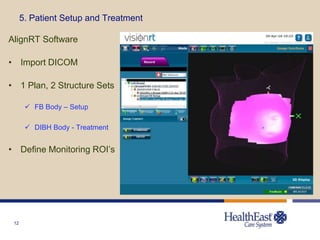
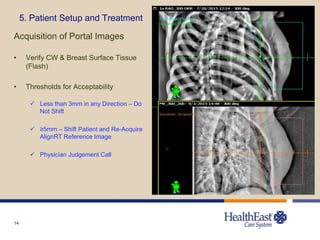
The document outlines the implementation of surface guided radiation therapy (SGRT) for left breast deep inspiration breath hold (DIBH) treatments, detailing practical considerations, system implementation, and patient treatment planning. Key elements include proper patient evaluation, equipment setup, and workflow to maximize reproducibility and treatment efficiency. The process is deemed scalable and effective, utilizing Varian TrueBeam and VisionRT technology.