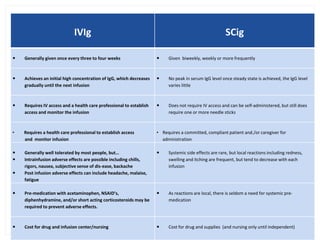
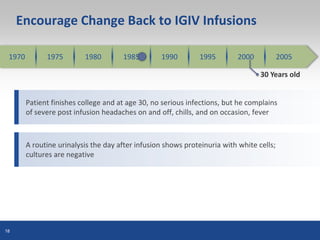
The document discusses the management of immunoglobulin replacement therapy, comparing intravenous immunoglobulin (IVIG) and subcutaneous immunoglobulin (SCIG) based on factors such as patient preferences, clinical outcomes, and side effects. It provides insights on dosing, troubleshooting, insurance issues, and presents clinical case histories illustrating the challenges and decisions in individualizing therapy for patients with immunodeficiency. Ultimately, the document emphasizes the need for personalized approaches in administering immunoglobulin therapy to enhance patient compliance and outcomes.