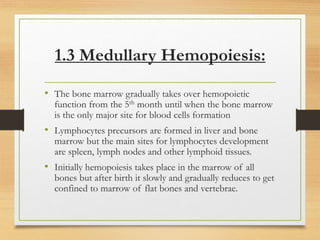
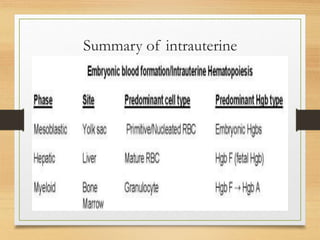
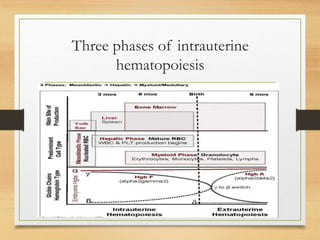
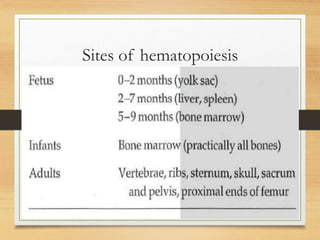
The document summarizes hematopoiesis, the formation of blood. It describes the three phases of intrauterine hematopoiesis that occur in different locations - the mesoblastic phase in the yolk sac, the hepatic phase in the liver, and the medullary phase in bone marrow. After birth, hematopoiesis occurs solely in the bone marrow. The bone marrow provides a microenvironment for blood cell formation through stromal cells, extracellular matrix, and growth factors. Hematopoietic precursors are divided into stem cells, progenitor cells, and maturing cells.