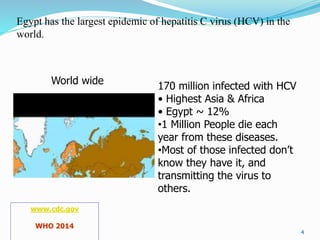
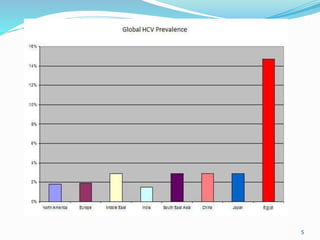
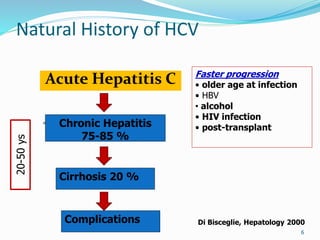
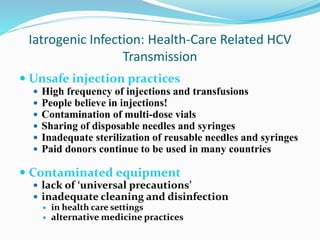
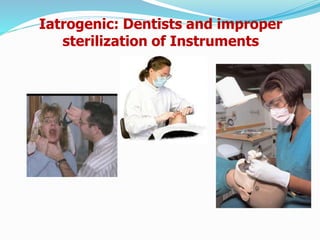
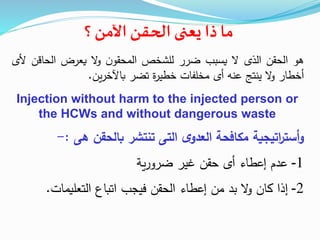
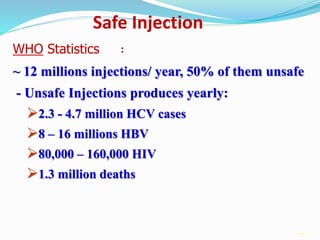
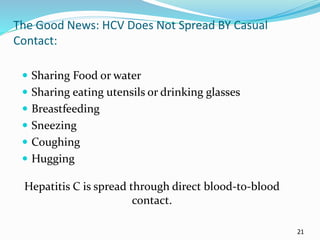
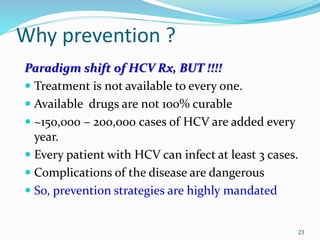
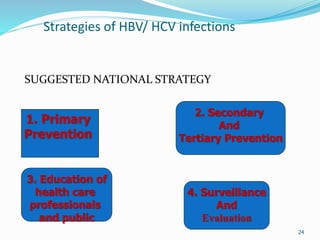
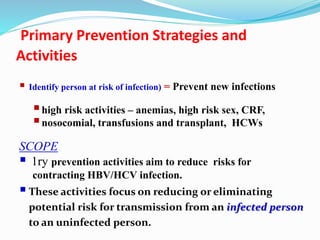
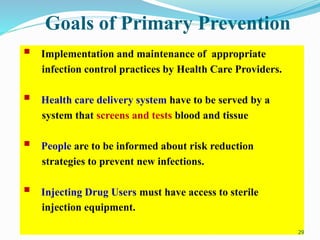
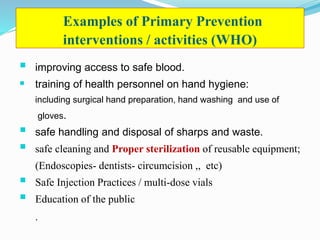
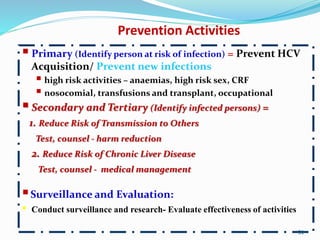
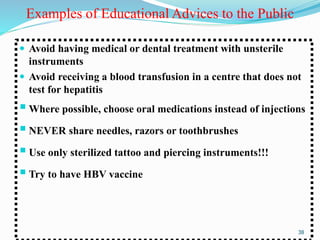
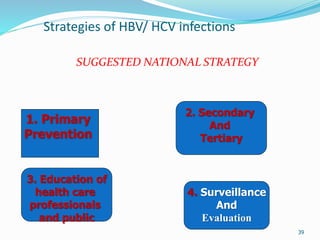
Egypt has the largest hepatitis C virus (HCV) epidemic in the world, with around 12% of the population infected. Unsafe injection practices from medical procedures are a major source of HCV transmission in Egypt. A suggested national HCV prevention strategy includes: 1) primary prevention through safe injection practices and infection control; 2) secondary prevention by identifying infected individuals and reducing transmission risk; 3) educating healthcare workers and the public; and 4) conducting surveillance and evaluating prevention activities. The strategy aims to prevent new HCV infections and reduce the risk of chronic liver disease in infected individuals through medical management and lifestyle changes.