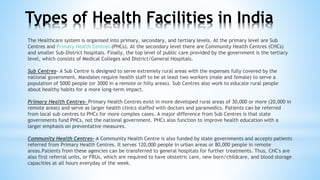
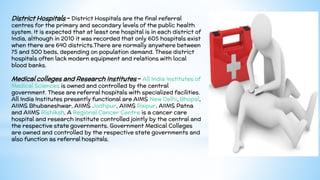
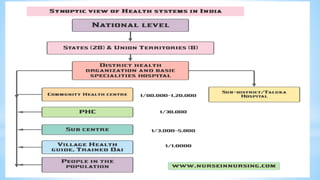
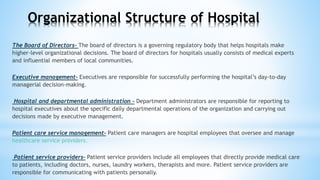
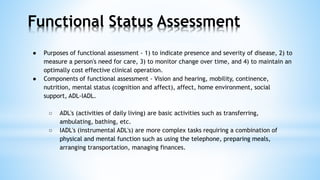
This document provides information about healthcare facilities in India. It discusses the primary, secondary, and tertiary levels of healthcare facilities. At the primary level are sub-centers and primary health centers. At the secondary level are community health centers and smaller sub-district hospitals. The tertiary level consists of medical colleges and district/general hospitals. It also outlines the organizational structure of hospitals and defines functional status of patients.