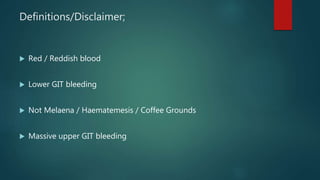
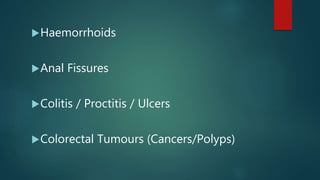
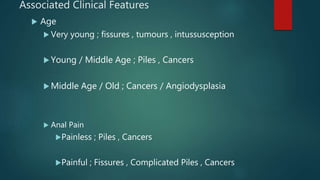
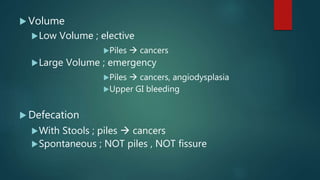
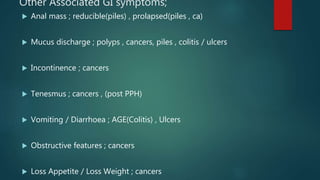
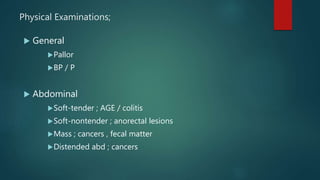
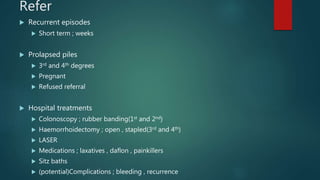
This document provides guidance for primary care physicians on evaluating and managing patients presenting with rectal bleeding. It outlines common causes of lower gastrointestinal bleeding including hemorrhoids, anal fissures, colitis, and colorectal tumors. Clinical features that help determine the likely cause are discussed. Evaluation involves assessing factors like age, pain, bleeding volume, defecation patterns, and physical examination. Treatment approaches for common conditions like hemorrhoids and anal fissures are described. Referral is recommended for recurrent, complicated, or higher risk cases to rule out more serious underlying issues.