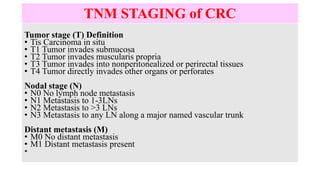
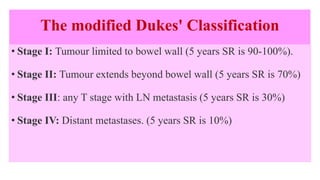
This document discusses colorectal cancer (CRC) examination, staging, investigations, and treatment. It covers CRC staging systems including TNM and Dukes' classification. Investigations include colonoscopy, CT, MRI, PET scans. Treatment involves surgical resection such as right hemicolectomy, low anterior resection, abdominoperineal resection. Adjuvant therapies include chemotherapy and chemoradiation. Prevention involves screening tests like FOBT, sigmoidoscopy, colonoscopy.