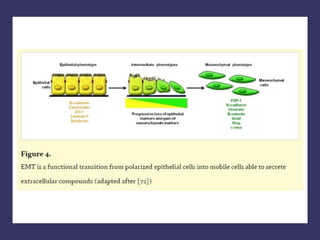
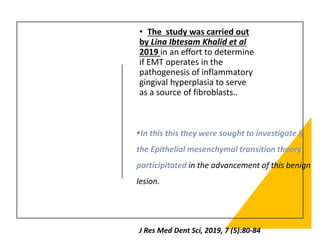
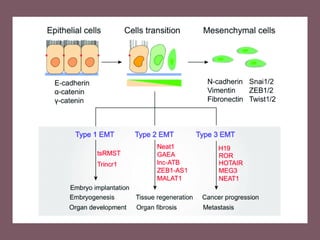
The document discusses the pathogenesis of gingival enlargement, emphasizing the role of epithelial-mesenchymal transition (EMT) in inflammatory gingival hyperplasia. It details the histological features and clinical implications of hereditary gingival fibromatosis, highlighting the transitions of epithelial cells into fibroblast-like cells and their effects on gingival health. Furthermore, it presents findings on immunohistochemical analyses of specific markers that support the involvement of EMT in the progression of this condition.
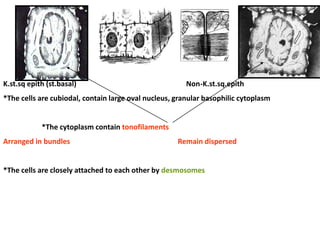
![Inflammatory gingival
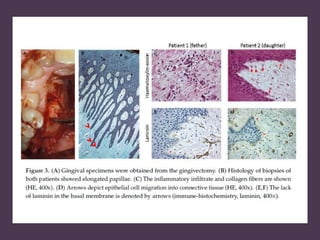
hyperplasia is an
inflammatory restraint
to local irritant
correlating with the
gingiva; the irritant
could be microbial like
plaque and calculus.
Clinically present as
deep red or bluish,
considerably friable and
fine with smooth glossy
surface and commonly
bleed easily [1].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-18-320.jpg)
![Gingival overgrowth usually
treated with traditional
periodontal treatment such as
scaling and root planning, but
if it include significant
fibrotic component that
don't respond to the
traditional treatment so it
will be treated by surgical
removal of the excess tissue
[3].
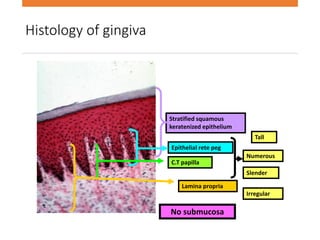
Histologically, inflammatory
gingival enlargement
characterized by thicking of
the epithelium with
increased volume of the
connective tissue with
different degree of
inflammation and fibrosis [2].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-19-320.jpg)
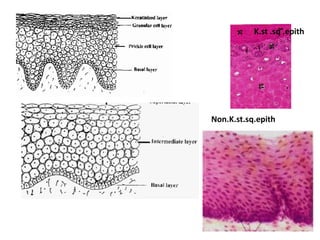
![• EMT is a process in which epithelial cells migrate
in to the connective tissue and transdifferentiate
into fibroblast-like cells, this occurs as the
epithelial cell-cell and cell- extracellular matrix
interactions are destabilized [4].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-21-320.jpg)






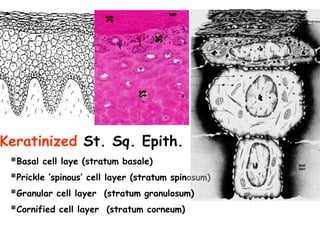
![Markers of the study:
E-Cadherin is considered as a
prototypical epithelial marker of
EMT.
Vimentin is mainly expressed in cells
of mesenchymal origin and it is
often used as a marker for
epithelial mesenchymal transition
Alpha smooth muscle actin positive
myofibroblast
E-Cadherin is required for the
maintenance of normal intercellular
adhesion and barrier integrity in
oral tissues [12].
Vimentin is one of the most familiar
members of intermediate filaments
(IFs), as it is the major IF protein in
mesenchymal cells and it is
frequently used as a developmental
marker of cells and tissues [13].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-58-320.jpg)
![The reduction in
epithelial expression of
E-Cadherin also called
the Cadherin switch has
been known to promote
EMT by facilitating
weakening of the
intercellular junctions
and promoting
movement of epithelial
cells towards the
connective tissue [6].
Alpha smooth muscle
actin positive
myofibroblast have
been demonstrated in
type 2 EMT [7].
To confirm this
mechanism, They
investigated the
Immuno-histochemical
expression of three
specific markers
assessing EMT
mechanism namely α-
SMA, Vimentin and E-
Cadherin.
Alpha-SMA is a putative
myofibroblast marker.
Since myofibroblasts are
implicated in EMT
induced fibrosis they
sought to analyse α –
SMA expression in the
samples.](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-59-320.jpg)

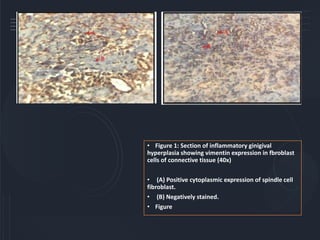
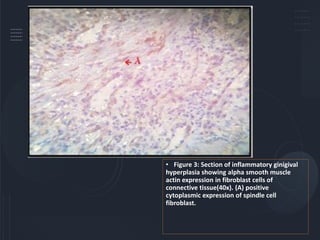
![Results:
The mean number of vimentin& E-Chadherin positive
fibroblast were 51.43% & 48.56%, respectively, so as these
two markers are biomarkers for EMT, it is suggested that
EMT process may be involved at least partly in the
pathogenesis of inflammatory gingival hyperplasia.
Vimentin and E-Chadherin immunoreactivity of the connective
tissue fibroblasts showed 100% positivity, while Alpha smooth
muscle actin staining was mostly seen in the endothelial
lined blood vessels with a few myofibroblast with in the
connective tissue being stained positive.
so increased expression and activation of TGF-B1 in
inflammatory gingival hyperplasia (14) promote an epithelial
cell plasticity that may progress to EMT [15].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-63-320.jpg)
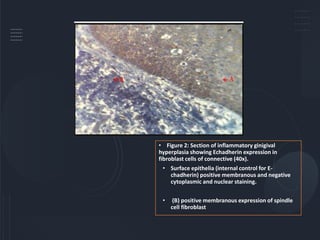
![Jeopardized E-Chadherin expression could alter the cell phenotype from
epithelial to fibroblast with spindle shape morphology [17].
Okada H and coworkers, (2000) have shown that the epithelial cells migrate
from the epithelial layer, travel through the basement membrane and
accumulate in the interstititium of the tissue; here they eventually get rid of
their epithelial markers and gain a fully fibroblastic phenotype [18,19].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-67-320.jpg)

![sometimes covering the entire crowns of the teeth and deforming the
palate, thereby creating occlusal and aesthetic problems, as well as causing
difficulties in speech and mastication.
Thickening of the alveolar ridge rarely appears at birth, typically initiates
with the eruption of deciduous or permanent dentition, exacerbates
during adolescence, and can persist within adulthood [1].
However radiographic imaging shows no specific changes in the teeth or
alveolar bone.](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-72-320.jpg)
![HGF may also exhibit an autosomal
dominant or recessive mode of
inheritance.
The recessive pattern usually linked to
other syndromes: Cowden, Jones,
Goltz-Gorlin,; and other systemic
diseases: cherubism, hypothyroidism,
chondrodystrophy, growth hormone
deficiency craniofacial dysmorphism or
leukemia [3–6].
Histologically, HGF shows gingival
features relatively acellular and with
an increased amount of randomly
arranged bundles of collagen.
The overlying epithelium may be
variable in thickness and have
prominent, elongated rete ridges
extending into the underlying
connective tissue [8].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-73-320.jpg)
![These conditions are presented with the epithelial to mesenchymal transition
(EMT), where the basal lamina show disruptions and epithelial cells migrate into
connective tissue and change their phenotypes to fibroblast-like cells [12].
However, these histological features are nonspecific, and the diagnosis should
be based on clinical findings and family history [11].
In rare cases, the description includes deposition of amyloids and islands of
odontogenic epithelium [10].](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-74-320.jpg)
![Fibroblasts are the key cells involved in the gingival production
of collagen and respond to the local stress depending on the
environmental conditions.
Therefore, is essential that they have to maintain a good
metabolic statement to respond to all aggressions.
Chronic Periodontitis is related to oxidative stress [14], and
previous studies have found a relationship between oxidative
stress and cyclosporine-induced gingival overgrowth [15], but to
date, no studies have linked this oxidative stress to HGF.](https://image.slidesharecdn.com/gingivalhyperplasia-240606093150-8e8c58e7/85/gingival-hyperplasia-underlying-Pathological-mechanisms-pdf-75-320.jpg)