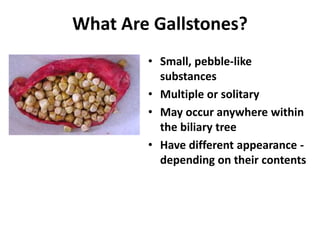
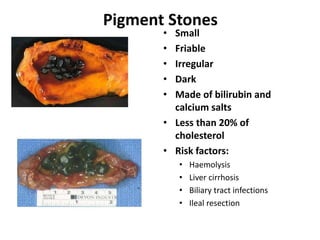
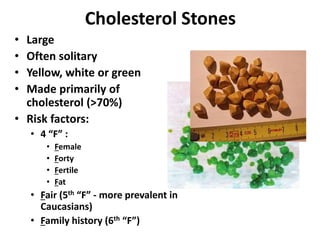
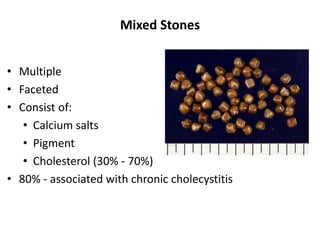
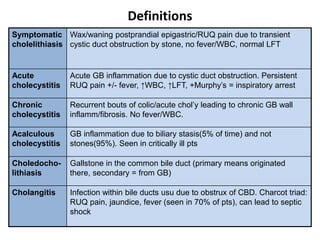
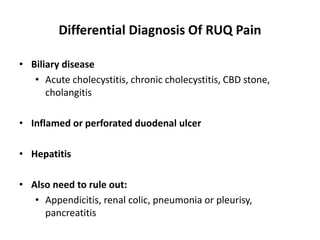
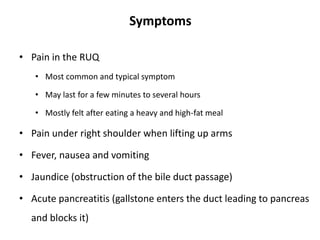
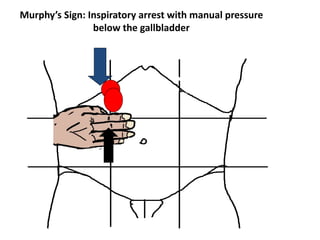
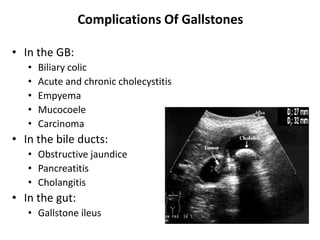
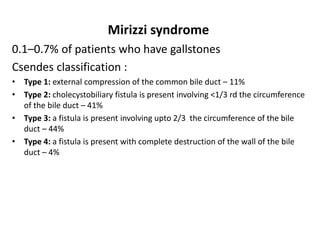
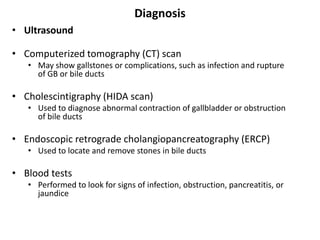
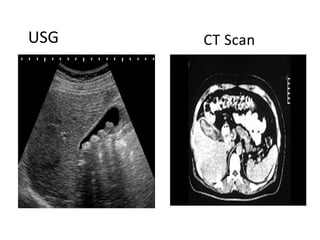
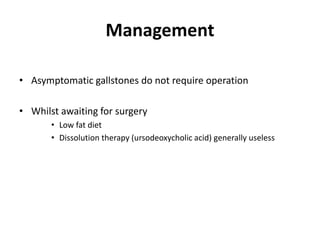
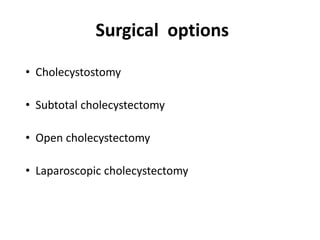
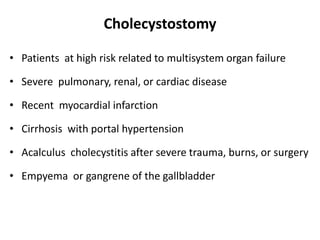
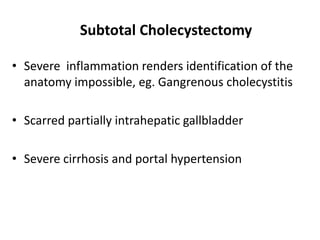
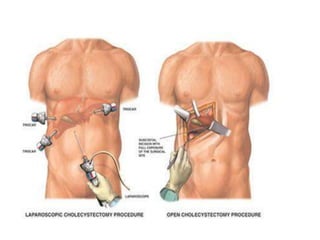
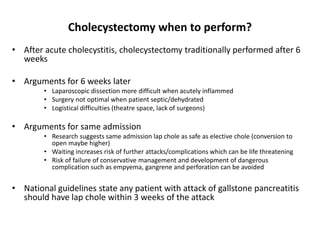
This document discusses gallstone disease including etiology, clinical features, diagnosis, and complications. It describes the different types of gallstones such as pigment stones, cholesterol stones, and mixed stones. Risk factors, symptoms, and potential complications are outlined. Diagnostic tools like ultrasound, CT scan, and HIDA scan are mentioned. Surgical options for gallstone treatment including cholecystostomy, subtotal cholecystectomy, open cholecystectomy, and laparoscopic cholecystectomy are summarized. Indications, procedures, and complications of cholecystectomy are also covered.