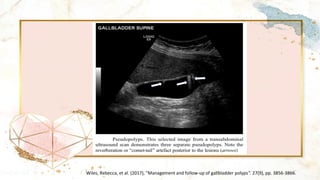
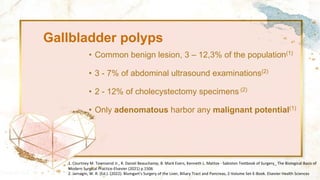
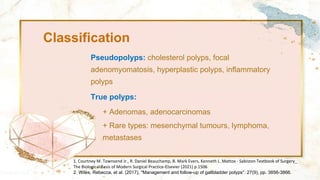
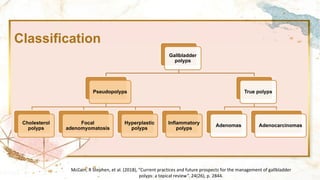
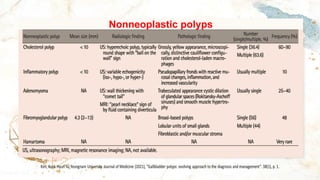
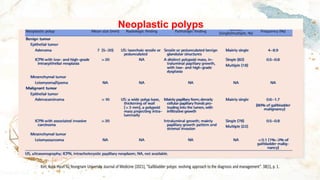
Gallbladder polyps are common benign lesions with a prevalence of 3-12% in the population and can pose a risk of malignancy, particularly adenomatous polyps. Various imaging techniques, including ultrasonography and endoscopic ultrasound, are used for diagnosis and follow-up, while management guidelines recommend cholecystectomy for polyps larger than 10 mm or if symptomatic. Most patients are asymptomatic, and follow-up strategies depend on the size and characteristics of the polyps.




![Radiological imaging
1. McCain, R Stephen, et al. (2018), "Current practices and future prospects for the management of gallbladder
polyps: a topical review". 24(26), p. 2844.]
2. Kim, Kook Hyun %J Yeungnam University Journal of Medicine (2021), "Gallbladder polyps: evolving approach
to the diagnosis and management". 38(1), p. 1.](https://image.slidesharecdn.com/gallbladderpolyps-240429074006-32f326a2/85/GALLBLADDER-POLYPS-di-u-tr-polyp-tui-m-t-pdf-16-320.jpg)