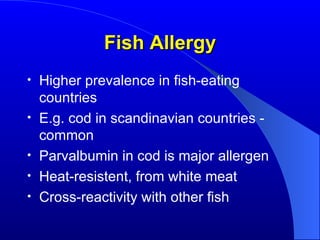
The document discusses food allergies, characterized as immunologic responses to specific food proteins, and highlights their prevalence, especially in young children. It enumerates common allergens, symptoms, diagnostic methods, and treatment approaches, emphasizing the importance of avoidance and good nutrition. Additionally, it outlines FDA regulations regarding allergen labeling and explores misconceptions about related conditions like celiac disease and 'leaky gut' syndrome.


![Prevalence of Food Allergies Highest in the first few years of life Declines over the first decade Never reaches zero People with other atopic diseases (allergic rhinitis [hay fever], atopic dermatitis [eczema], asthma) are MORE likely to have food allergies also 35% more likely in moderate to severe eczema](https://image.slidesharecdn.com/food-allergy-1230341390732425-2/85/Food-Allergy-4-320.jpg)