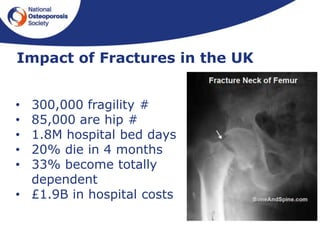
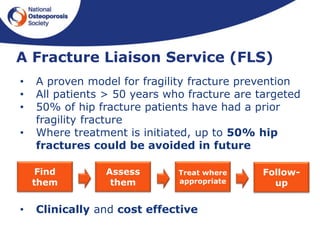
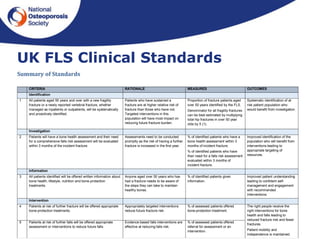
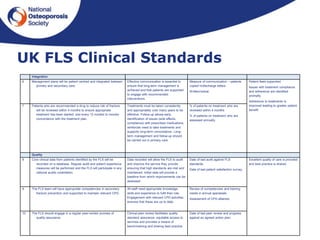
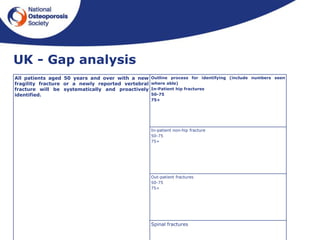
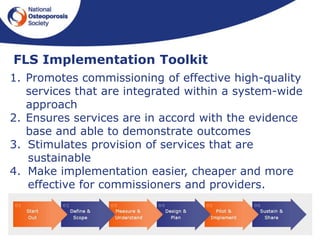
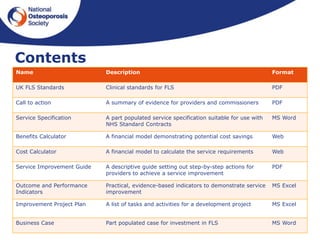
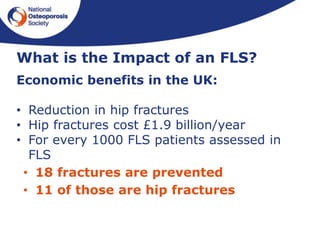
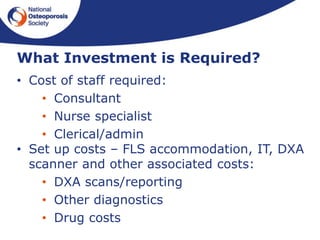
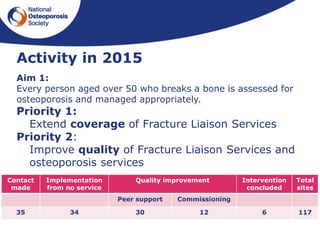
This document outlines the National Osteoporosis Society's plans to implement Fracture Liaison Services (FLS) across the UK. FLS aim to systematically identify, assess, and treat patients over 50 who have experienced fragility fractures to reduce their risk of future fractures. The document discusses establishing an FLS Implementation Group to provide strategic leadership. It also outlines developing UK FLS Clinical Standards, an FLS Implementation Toolkit, and training to help establish high quality FLS nationally. The goal is to have every person over 50 who breaks a bone assessed for osteoporosis and managed appropriately through an FLS approach.