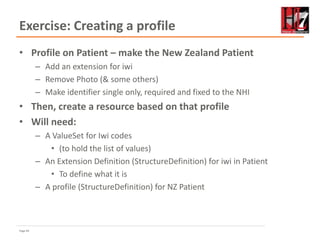
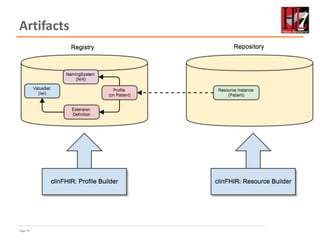
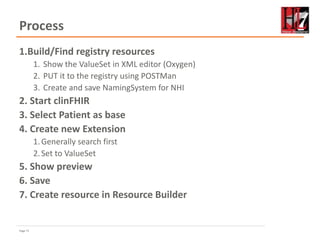
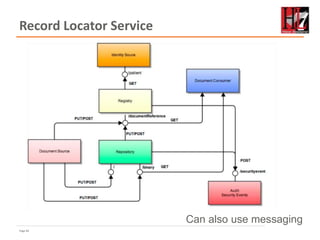
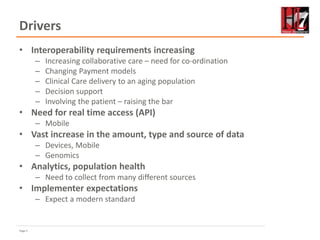
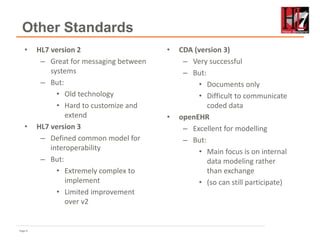
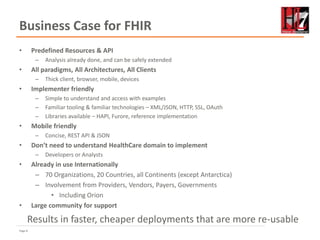
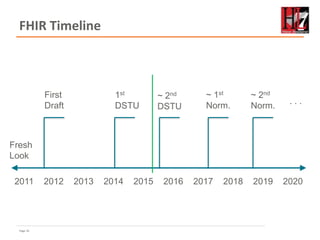
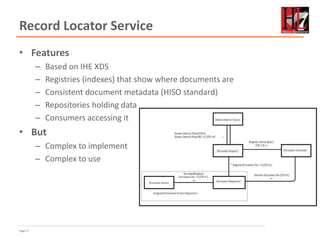
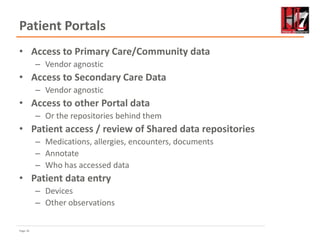
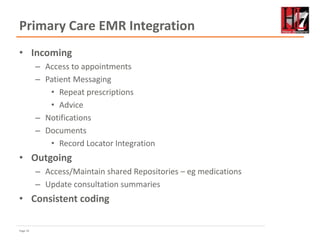
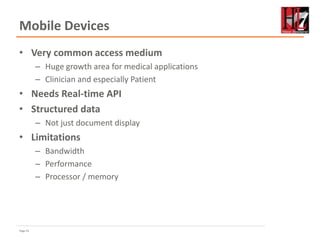
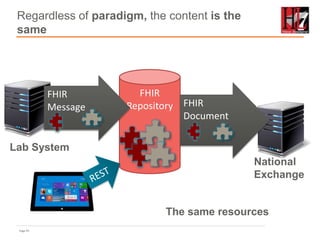
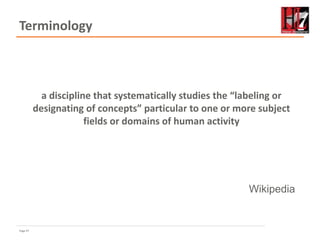
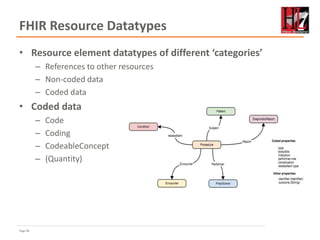
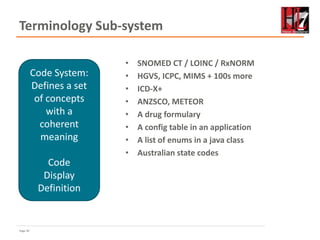
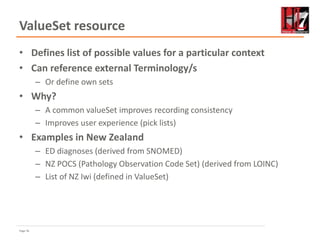
This document provides an overview of FHIR (Fast Healthcare Interoperability Resources) and its potential uses in New Zealand. It discusses drivers for adopting FHIR like increasing data sharing needs, the limitations of current standards, and how FHIR addresses these through resources, APIs, terminology support and other features. The document outlines FHIR concepts like resources, paradigms for exchange, and use of terminology systems. It proposes several potential early uses of FHIR in New Zealand like patient portals, primary care integration, mobile apps and a record locator service. The presentation aims to show attendees where FHIR fits in New Zealand and encourage further learning and planning pilots.







![Page 42
FHIR RESTful Interactions
• Instance
– Read GET [base]/Patient/100
– Vread GET [base]/Patient/100/{vid}
– Update PUT [base]/Patient/100
– Delete DELETE [base]/Patient/100
– History GET [base]/Patient/100/_history
• Type
– Create POST [base]/Patient
– Search GET [base]/Patient?name=eve
– History GET [base]/Patient/_history
– Validate POST [base]/Patient/100/_validate/{id}
• System
– Conformance GET [base]/metadata
– Transaction POST bundle to root
– History GET [base]/_history
– Search GET [base]/Patient?name=eve](https://image.slidesharecdn.com/hl7nz-v3-150724082900-lva1-app6891/85/FHIR-Ice-36-320.jpg)

![Page 49
Examples
• Code: "status" : "confirmed"
• Coding: {
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "C3214954",
"display": "cashew nut allergenic extract Injectable"
}
• CodeableConcept: {
"coding": [{
"system": "http://snomed.info/sct",
"code": "39579001",
"display": "Anaphylactic reaction“
}],
"text" : "Anaphylaxis"
}](https://image.slidesharecdn.com/hl7nz-v3-150724082900-lva1-app6891/85/FHIR-Ice-43-320.jpg)
![Page 54
NamingSystem resource
• A coded element needs to
indicate the terminology
– How to know which ‘system’
value to use?
• Some standard ones defined
in the spec
– SNOMED, LOINC etc.
• Other datatypes need the
same
– Identifier
• Can define own ones
– Using NamingSystem resource
– uniqueId is key
{
"resourceType": "NamingSystem",
"id": "nznhi",
"meta": {
"versionId": "2",
"lastUpdated": "2015-07-21T19:58:39Z"
},
"text": {
"status": "generated",
"div": "<div xmlns="http://www.w3.org/1999/xhtml">New Zealand
NHI</div>"
},
"type": "identifier",
"name": "NZ NHI",
"date": "2014-12-13",
"status": "active",
"description": "The New Zealand NHI system",
"uniqueId": [
{
"type": "uri",
"value": "http://hl7.org.nz/ns/nhi"
}
],
"contact": [
{
"telecom": [
{
"system": "email",
"value": "nhiteam@moh.co.nz"
}
]
}
]
}](https://image.slidesharecdn.com/hl7nz-v3-150724082900-lva1-app6891/85/FHIR-Ice-48-320.jpg)
![Page 57
ValueSet for condition.code
{
"resourceType": "ValueSet",
"id": "valueset-condition-code",
"meta": {
"versionId": "1",
"lastUpdated": "2015-05-08T16:18:23Z",
},
"text": {
"status": "generated",
"div": ”Condition.code sample ValueSet"
},
"url": "http://hl7.org/fhir/vs/condition-code",
"version": "0.5.0",
"name": "Condition/Problem/Diagnosis Codes",
"publisher": "FHIR Project team",
"contact": [
{
"telecom": [
{
"system": "url",
"value": "http://hl7.org/fhir"
}
]
}
],
"description": "Example value set for
Condition/Problem/Diagnosis codes",
"copyright": "This value set includes content
from SNOMED CT, which is copyright © 2002+
International Health Terminology Standards
Development Organisation (IHTSDO), and
distributed by agreement between IHTSDO and
HL7. Implementer use of SNOMED CT is not
covered by this agreement",
"status": "draft",
"experimental": true,
"compose": {
"include": [
{
"system": "http://snomed.info/sct",
"filter": [
{
"property": "concept",
"op": "is-a",
"value": "404684003"
}
]
}
]
}
}](https://image.slidesharecdn.com/hl7nz-v3-150724082900-lva1-app6891/85/FHIR-Ice-51-320.jpg)
![Page 58
Valueset for NZ Iwi
{
"resourceType": "ValueSet",
"id": "nziwi",
"meta": {
"versionId": "4",
"lastUpdated": "2015-07-18T19:29:40Z"
},
"text": {
"status": "generated",
"div": "<div xmlns="http://www.w3.org/1999/xhtml">

<p>Valueset for Iwi</p>
 </div>"
},
"url": "http://fhir-dev.healthintersections.com.au/open/ValueSet/nziwi",
"version": "1",
"name": "New Zealand Iwi",
"publisher": "HL7 New Zealand",
"contact": [ {
"telecom": [
{
"system": "email",
"value": "david.hay25@gmail.com"
}
]
} ],
"description": "The list of possible Iwi (tribes) for New Zealand",
"requirements": "Needed for an extension on Patient",
"status": "draft",
"experimental": true,
"date": "2015-06-13",
"define": {
"system": "fhir.hl7.org.nz/valueset/nziwi",
"concept": [
{
"code": "kt",
"display": "Kai Tahu"
},
{
"code": "np",
"display": "Ngāti Porou"
},
{
"code": "nt",
"display": "Ngāi Tahu"
},
{
"code": "np1",
"display": "Ngā Puhi"
},
{
"code": "nk",
"display": "Ngāti Kahungunu"
},
{
"code": "th",
"display": "Tūhoe"
}
]
}
}](https://image.slidesharecdn.com/hl7nz-v3-150724082900-lva1-app6891/85/FHIR-Ice-52-320.jpg)