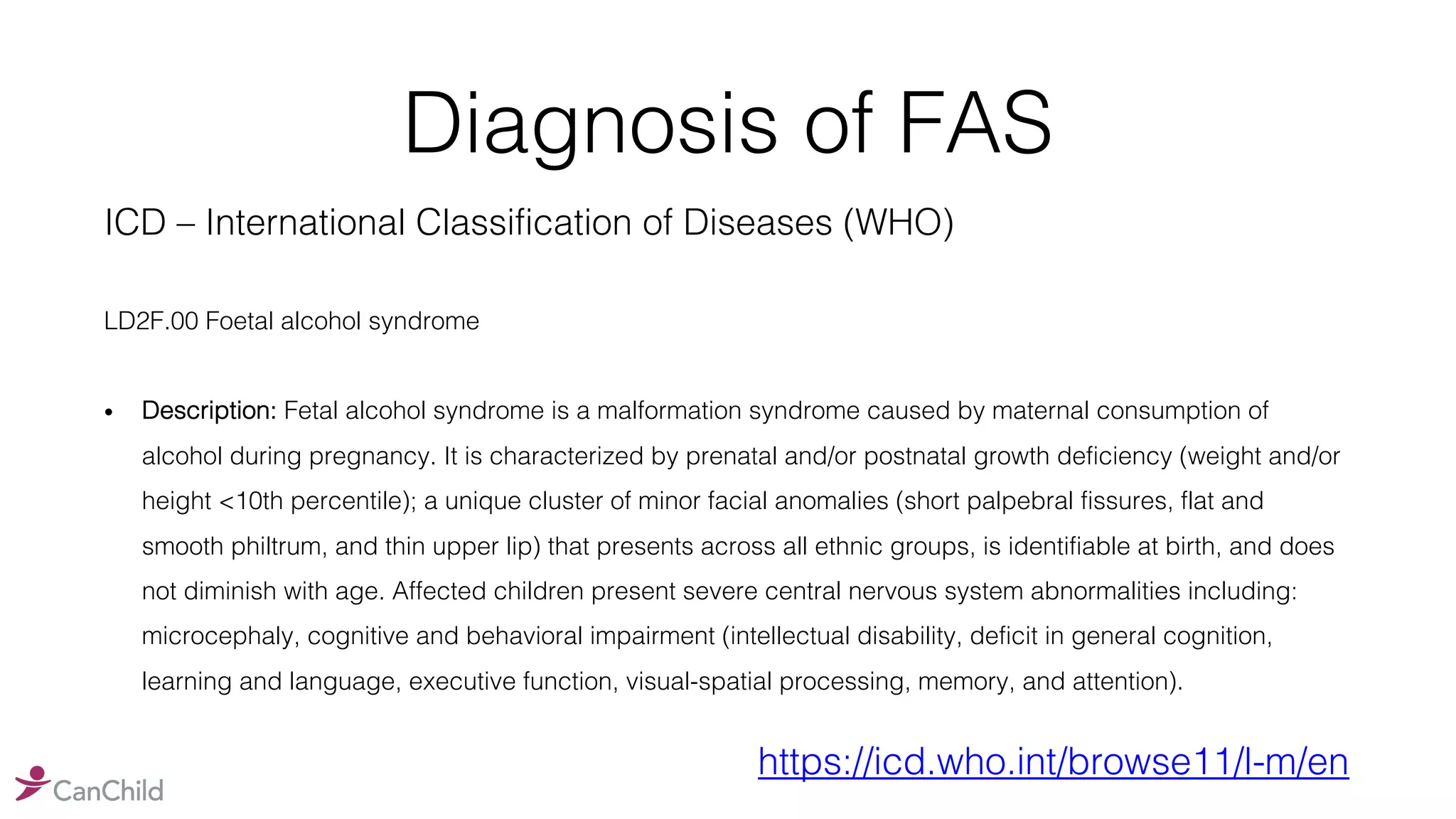
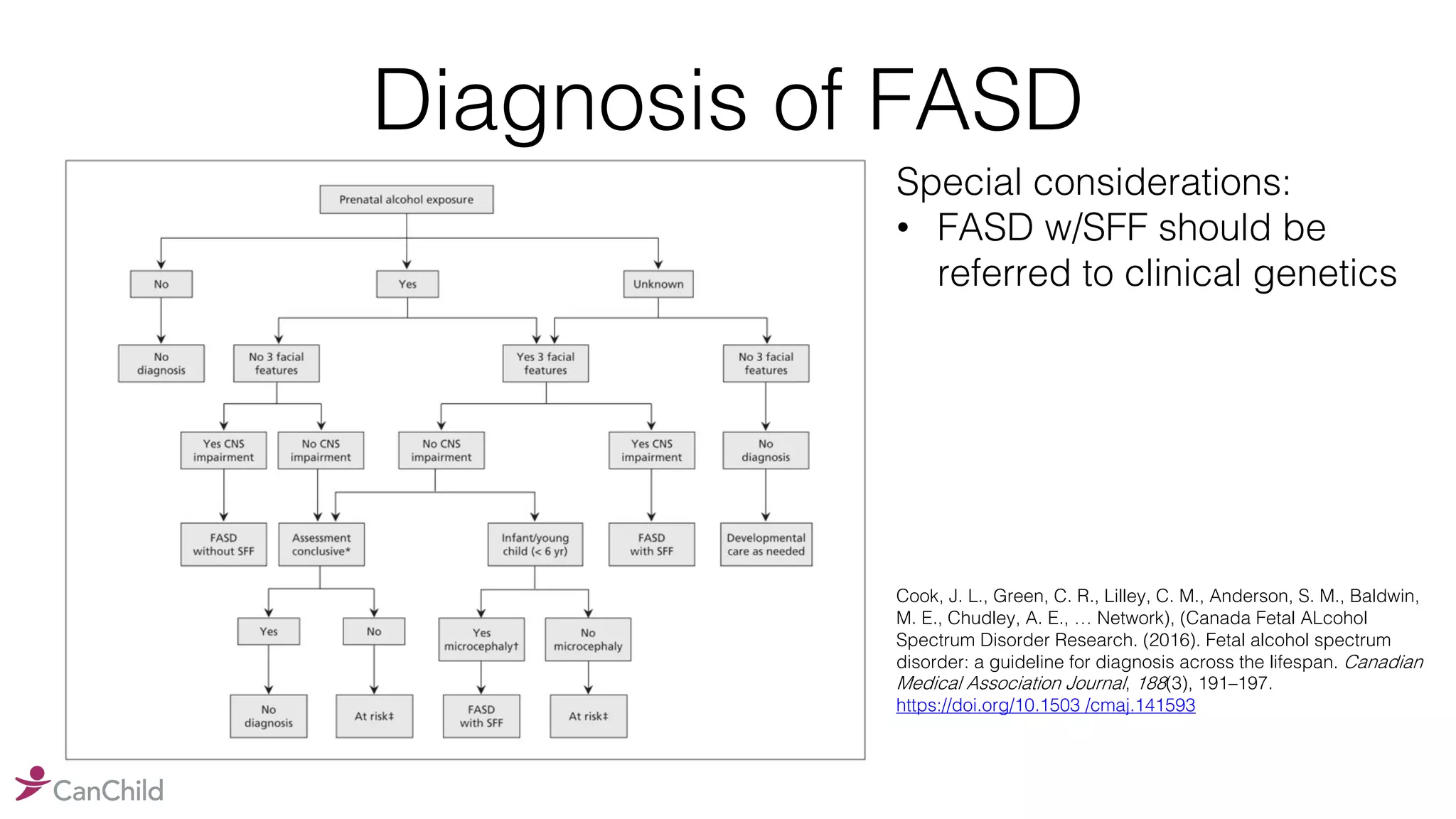
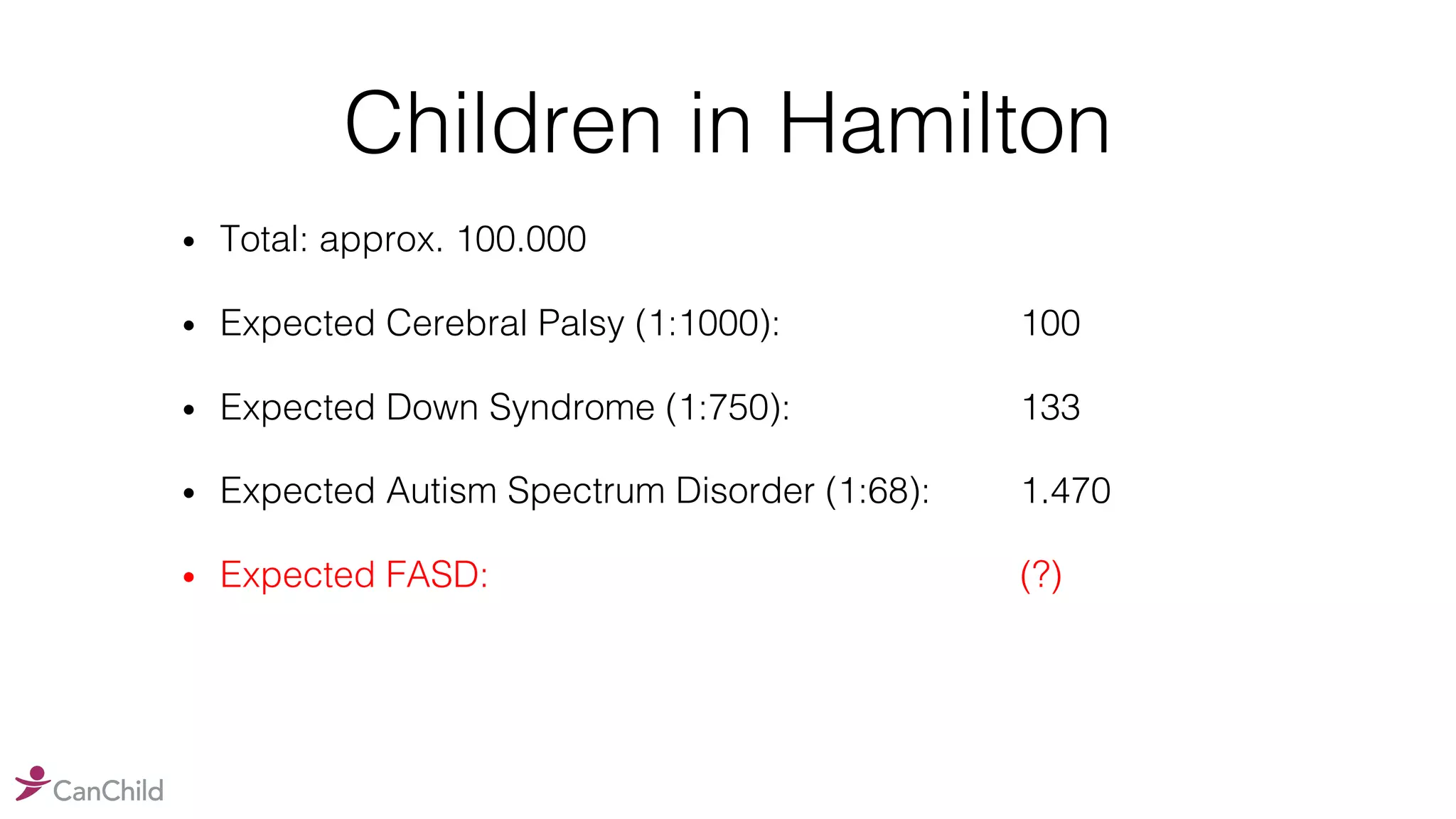
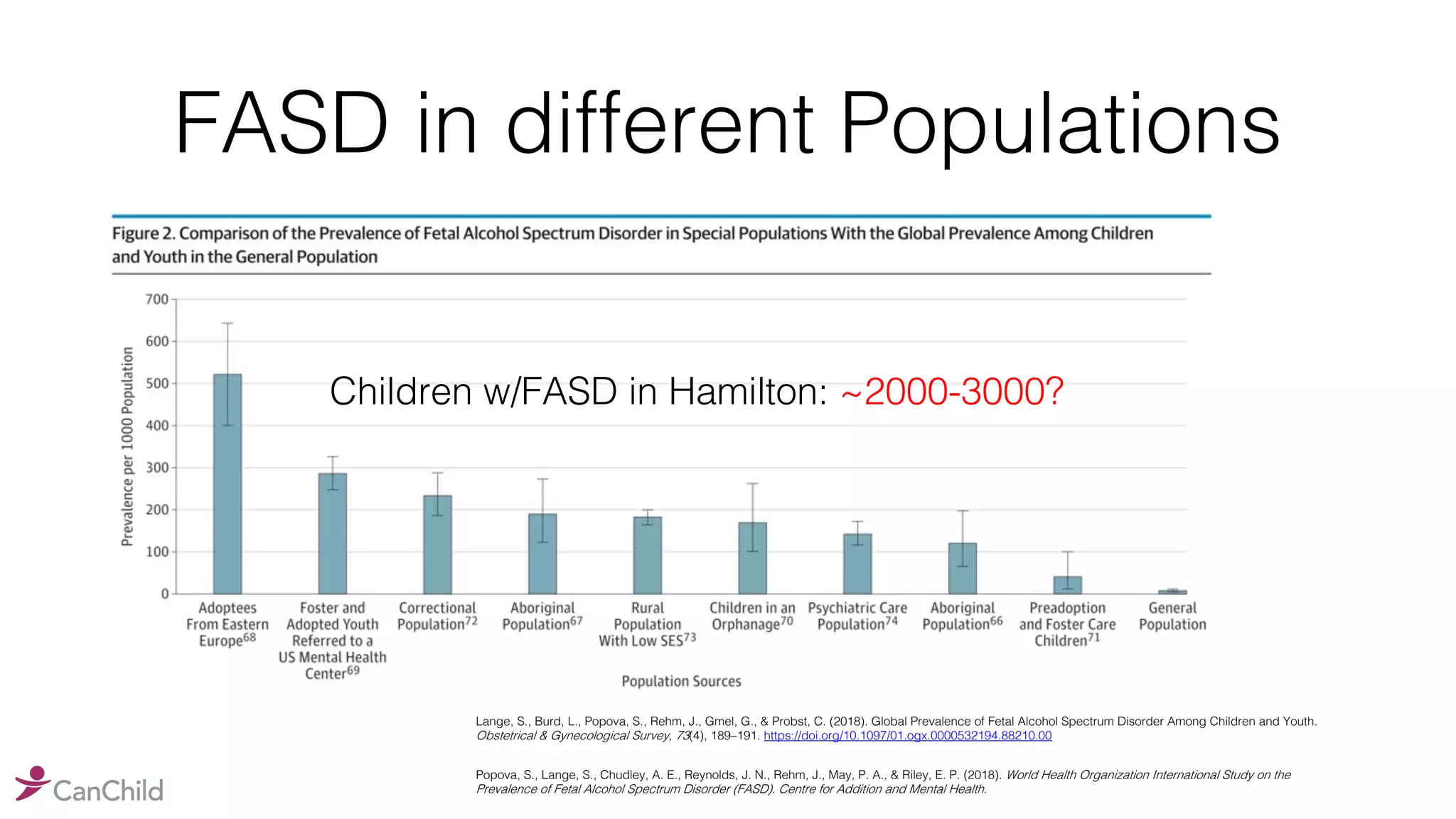
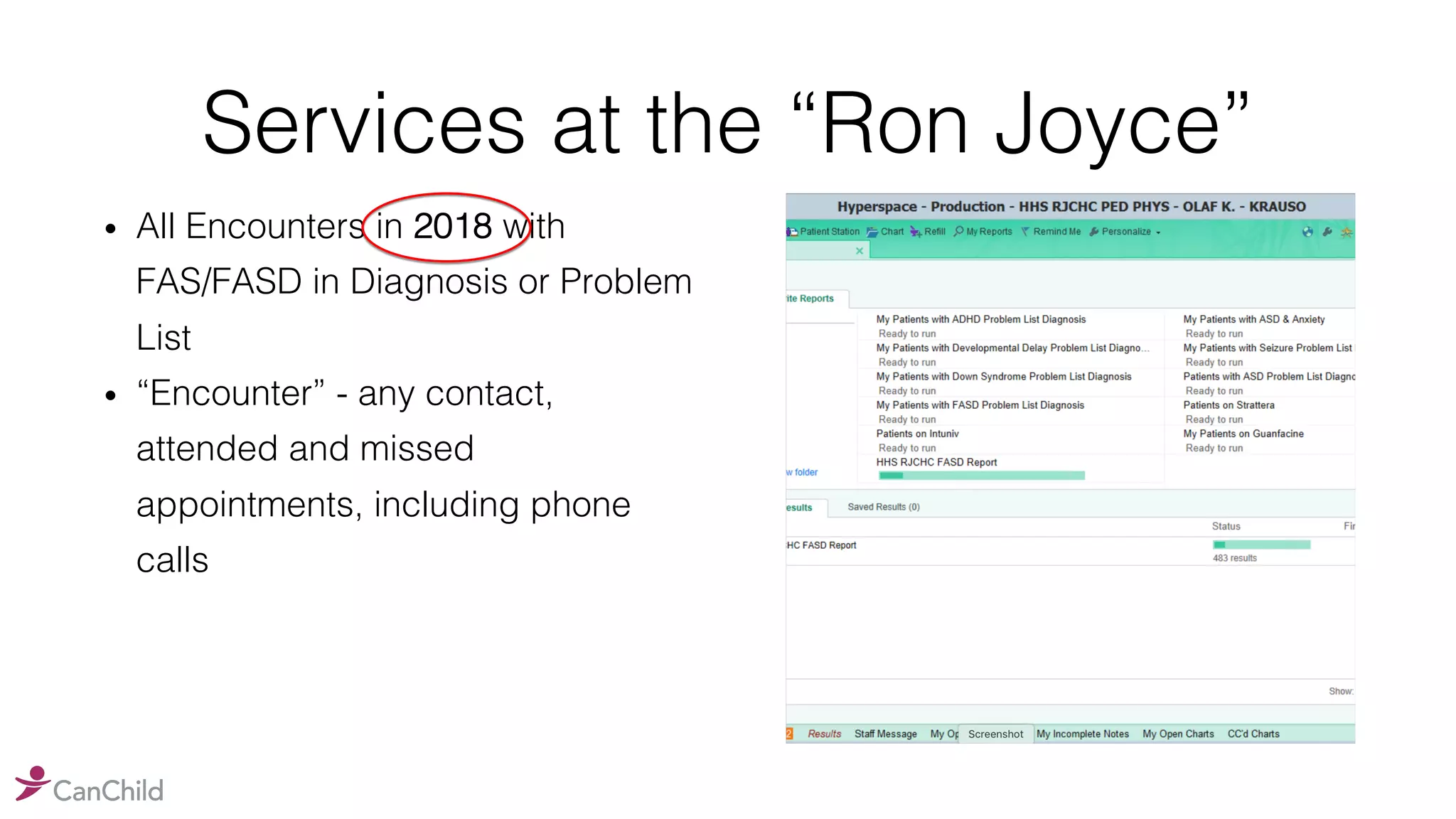
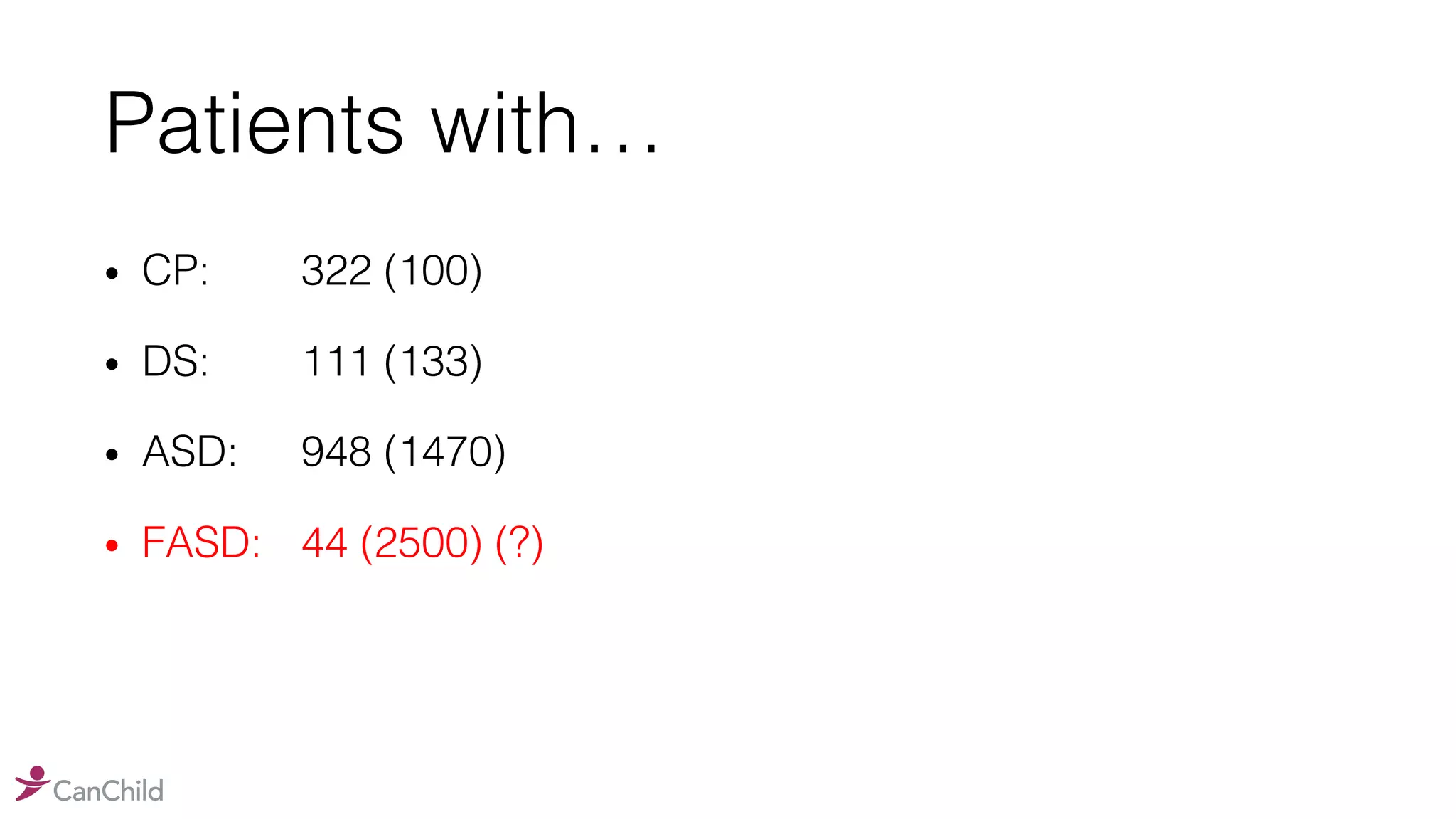
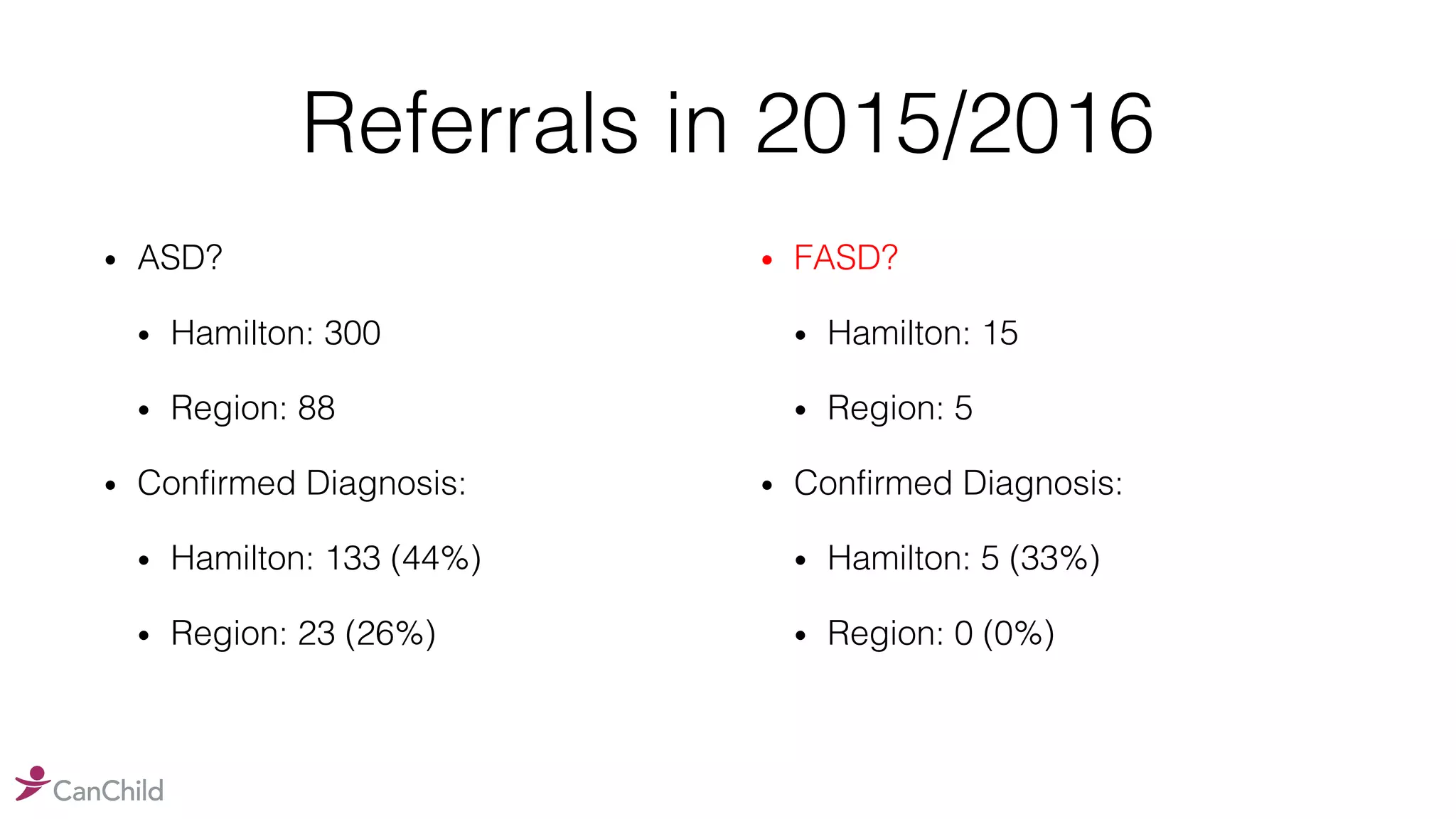
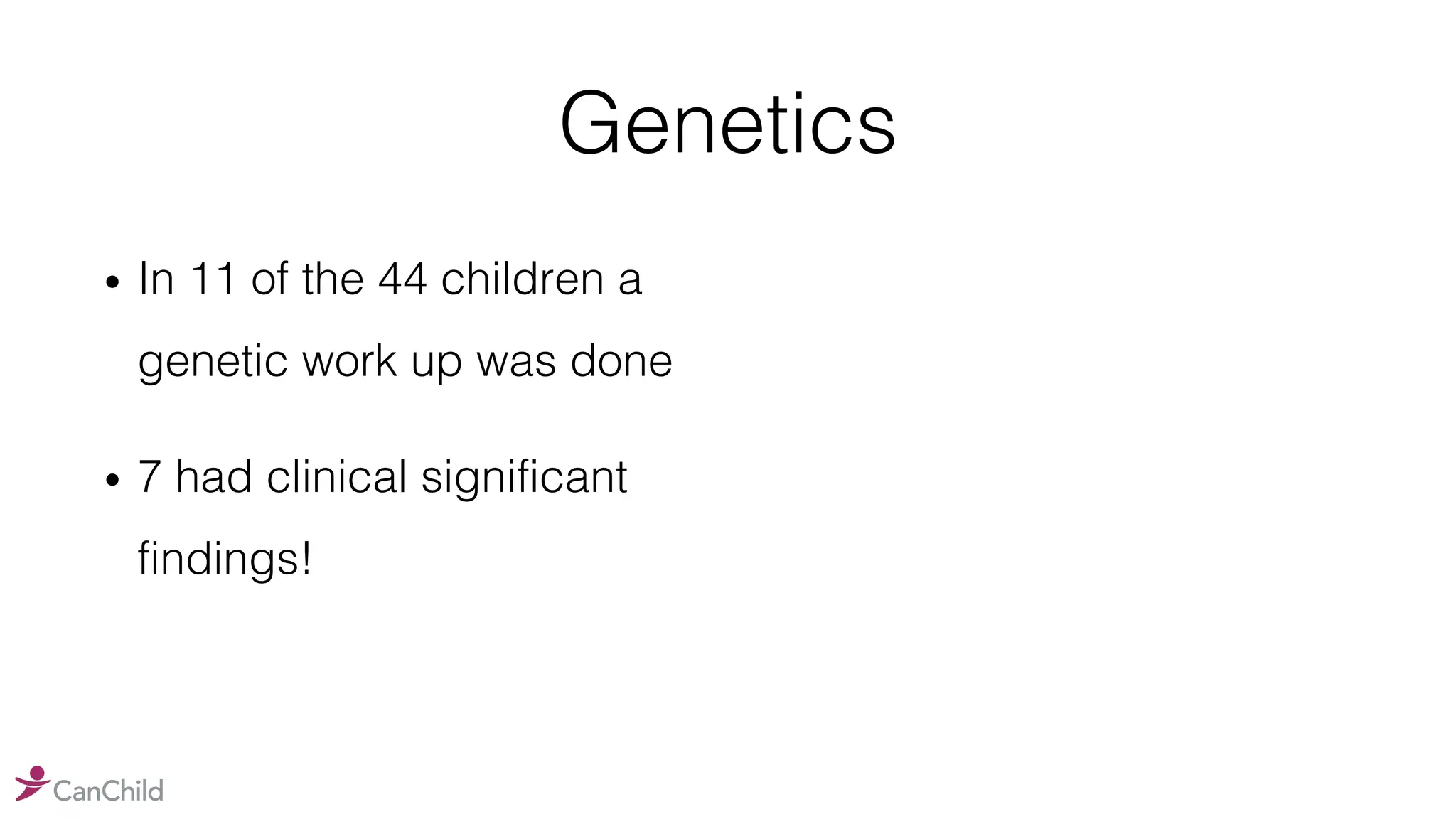
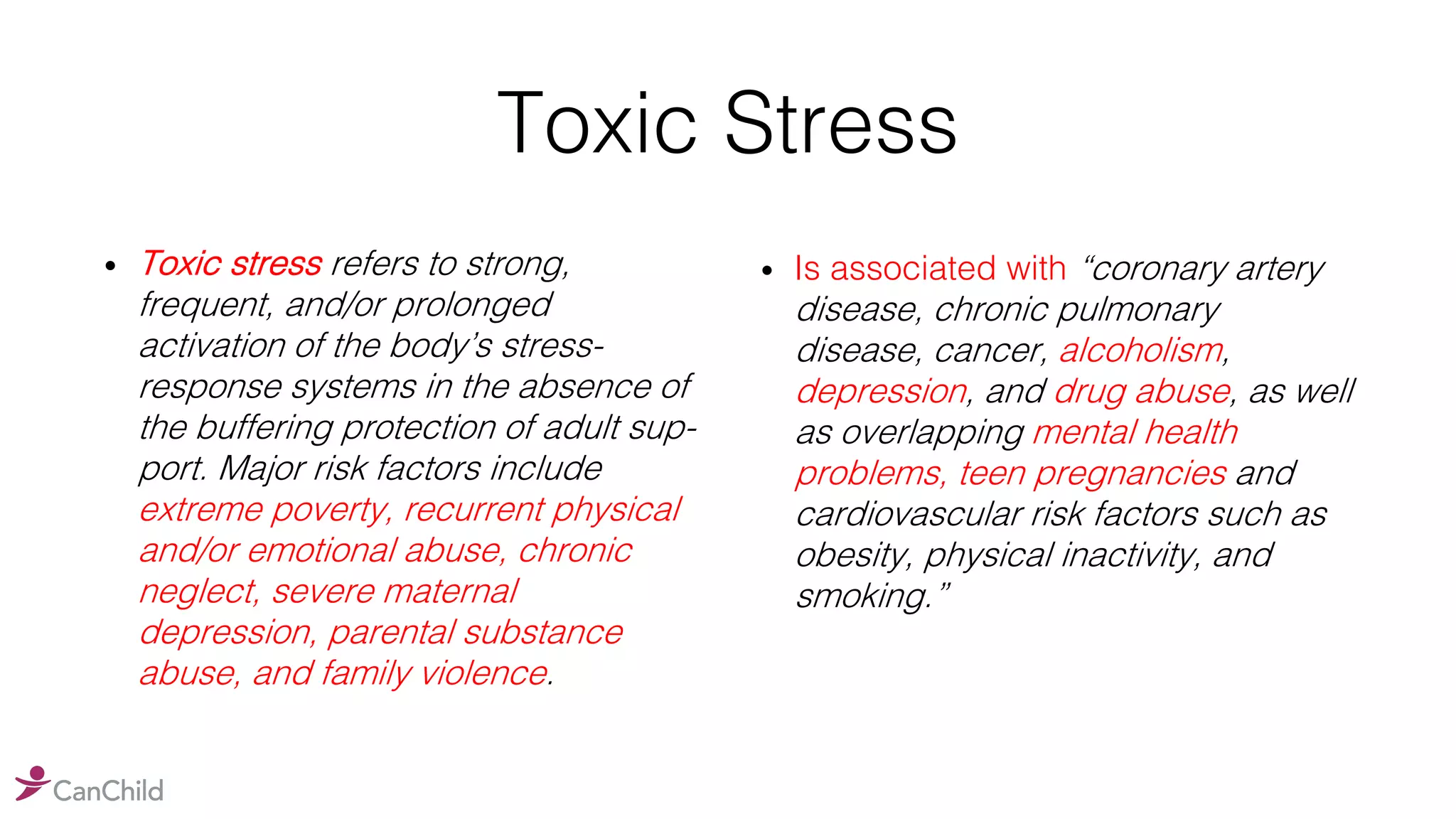
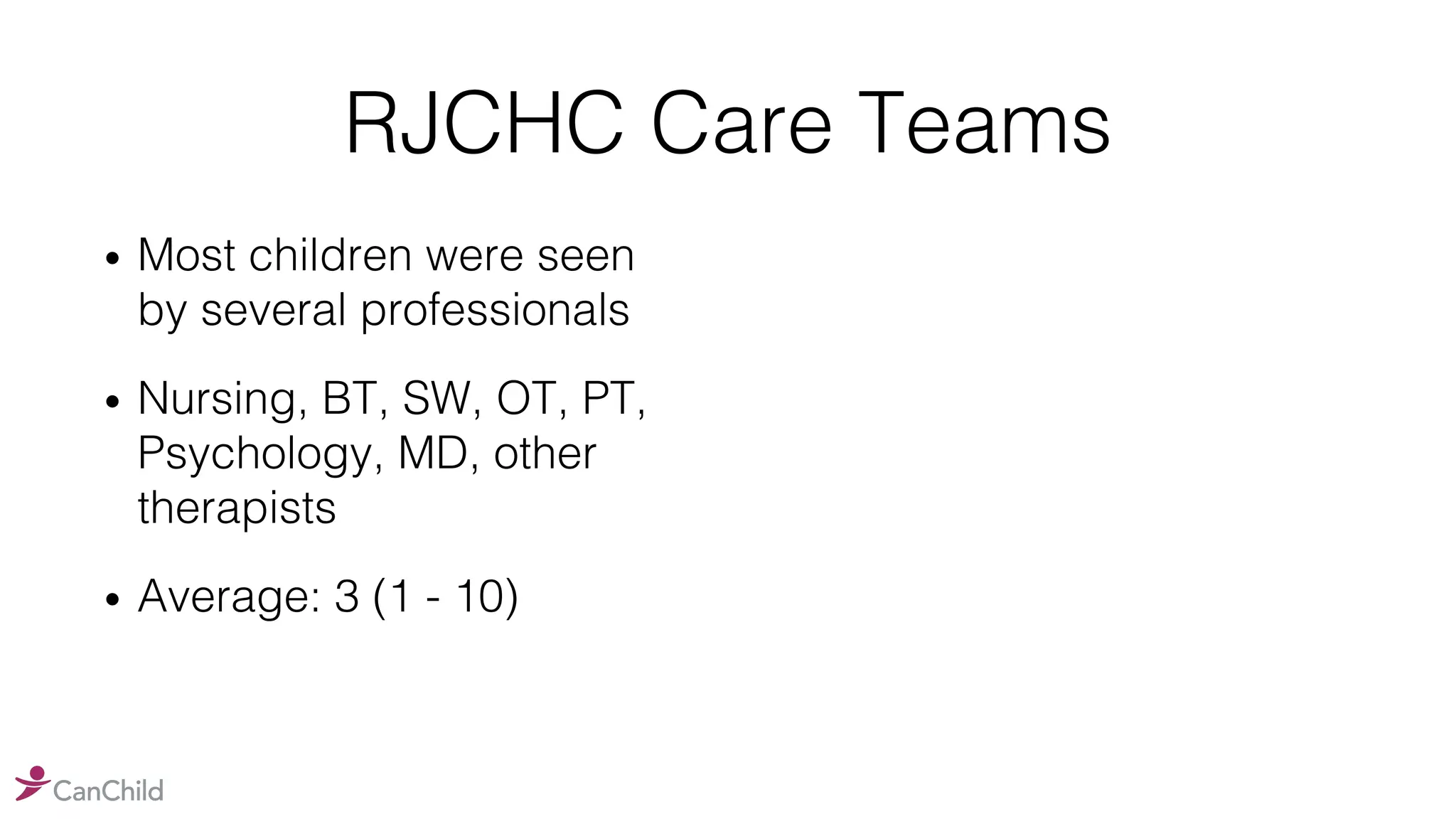
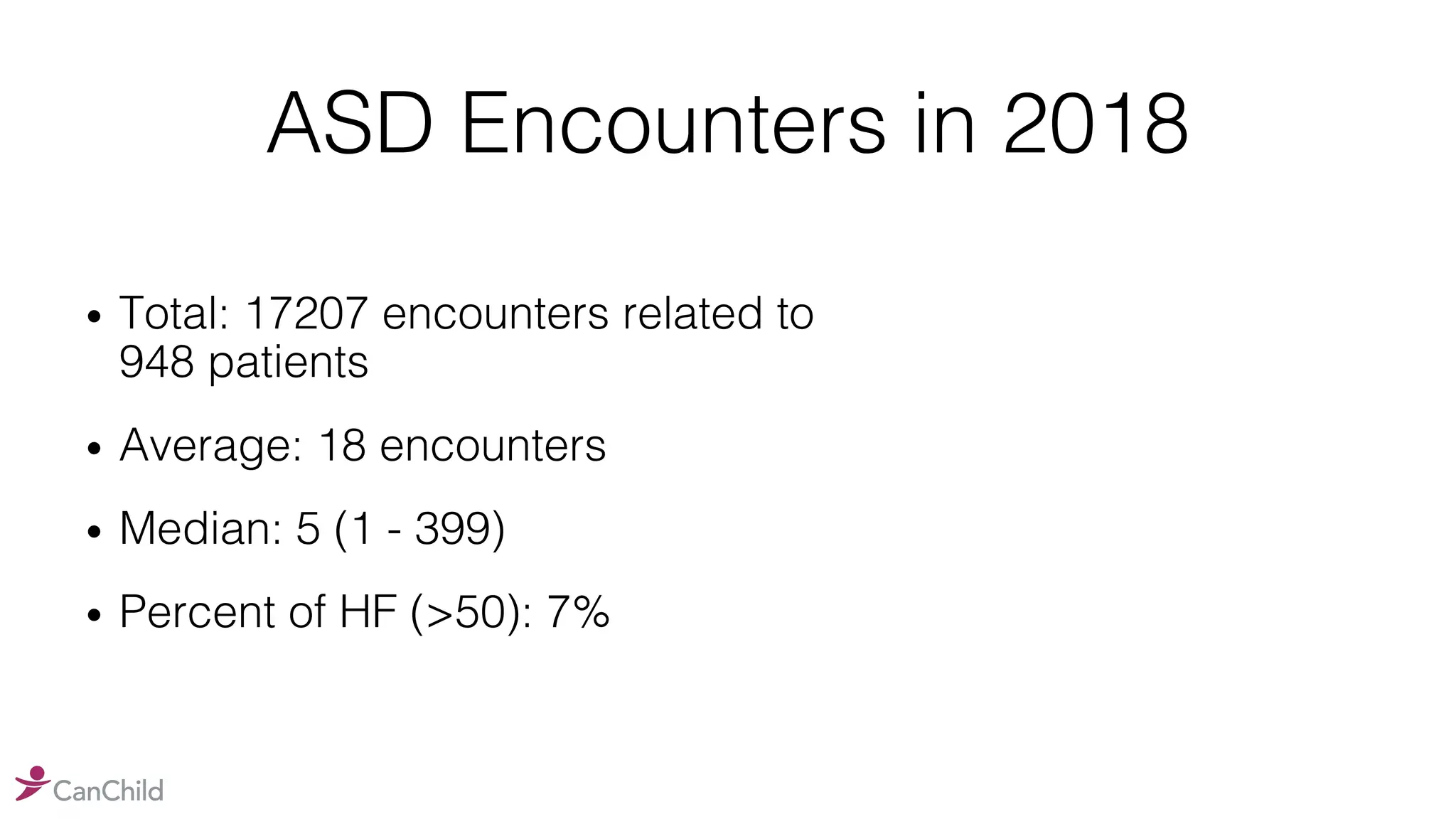
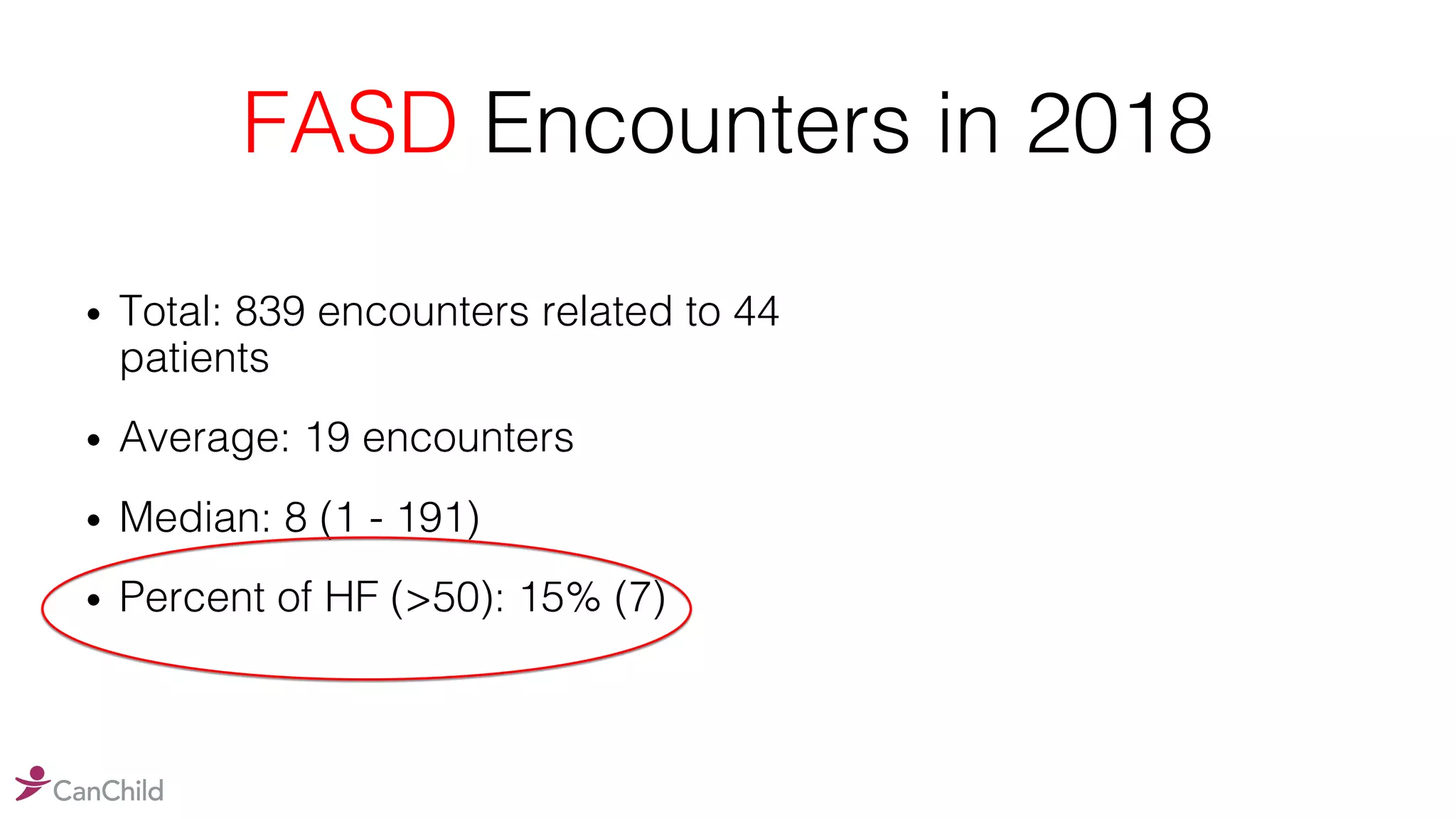
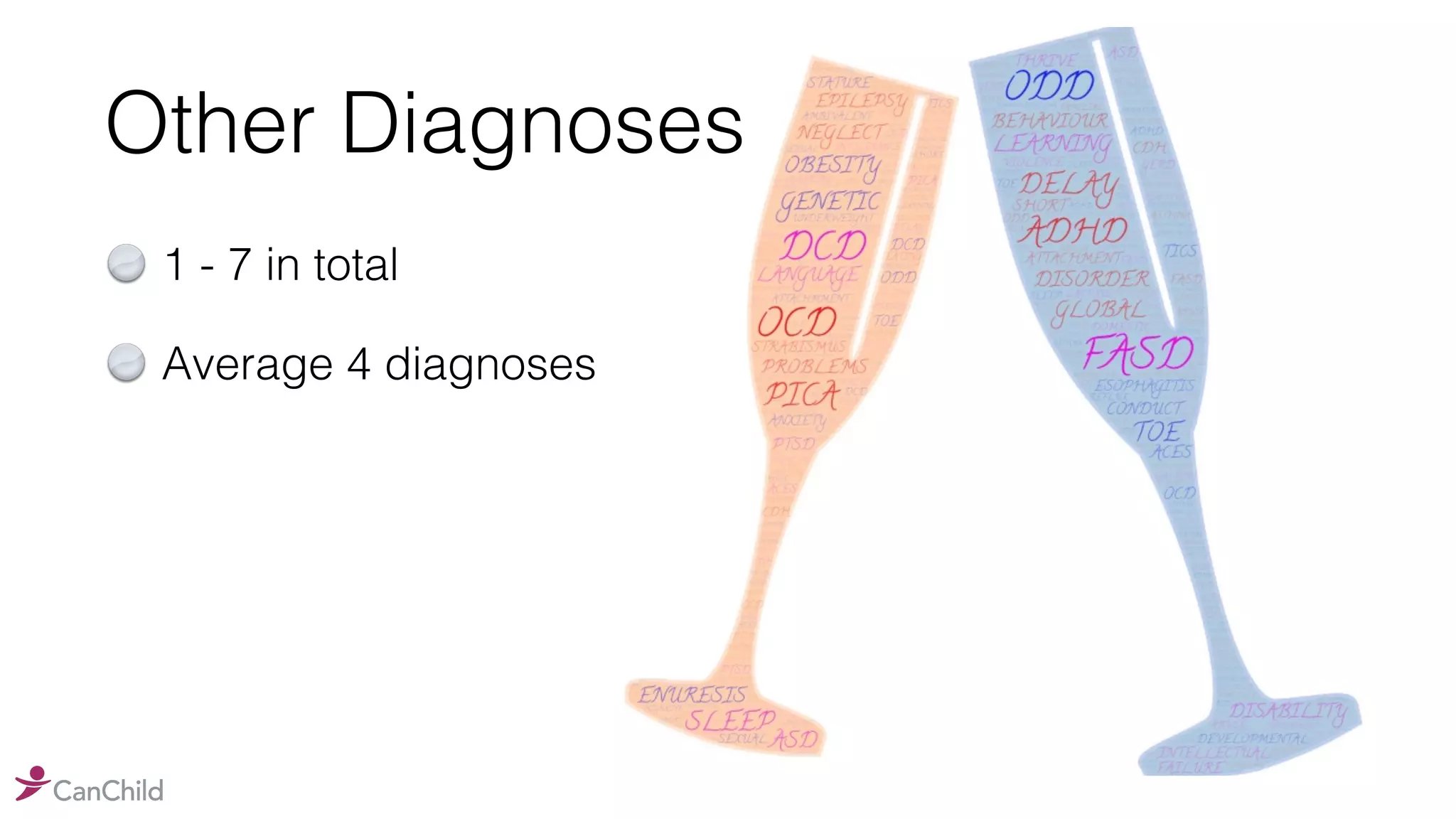
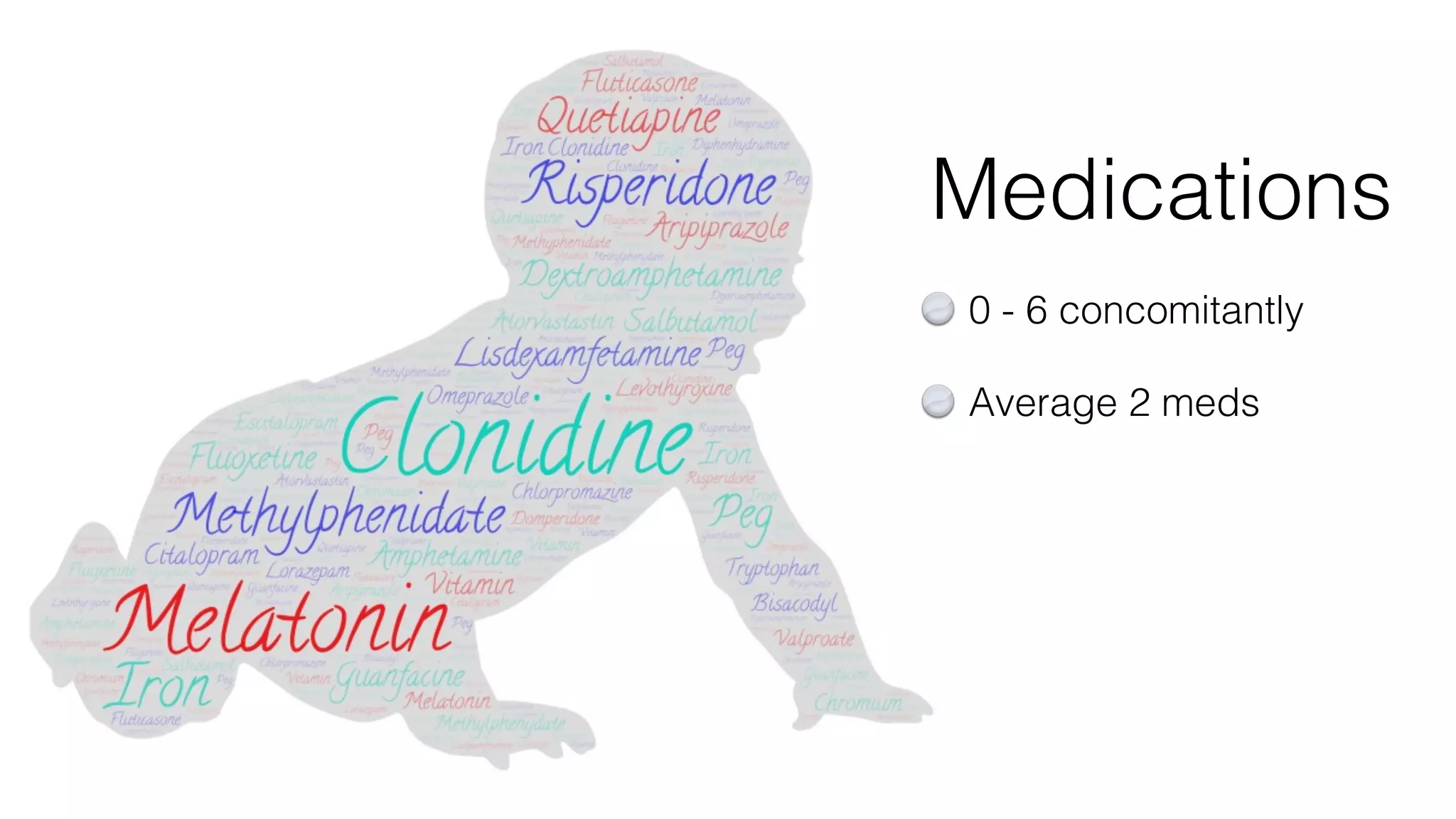
The document discusses the diagnosis and treatment of fetal alcohol spectrum disorder (FASD) in Hamilton, emphasizing the need for a multi-professional team approach to address the developmental challenges faced by affected children. It highlights a low referral rate and low community awareness, as well as the significant prevalence of genetic abnormalities among children with neurodevelopmental disabilities. The importance of tailored supports and comprehensive assessments to improve outcomes for these children is also outlined.