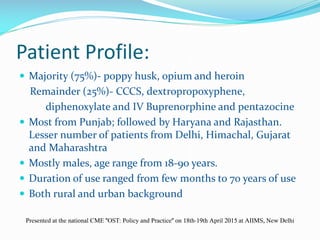
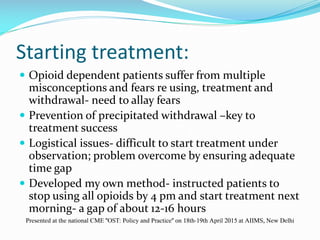
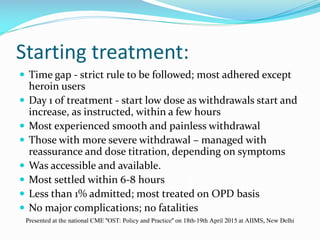
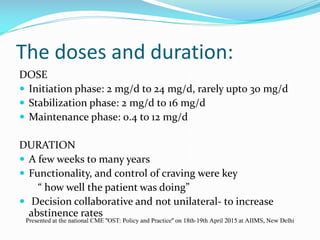
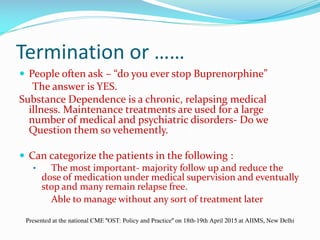
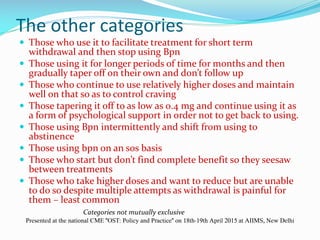
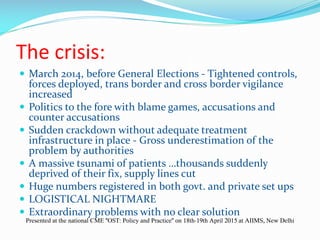
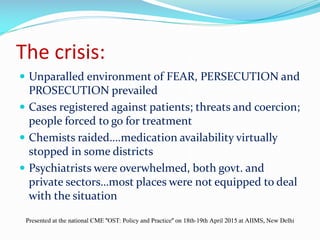
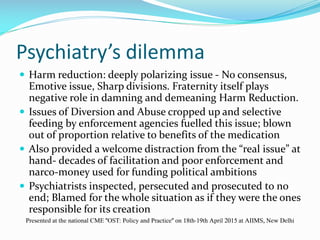
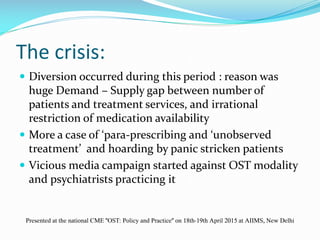
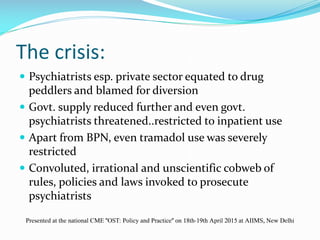
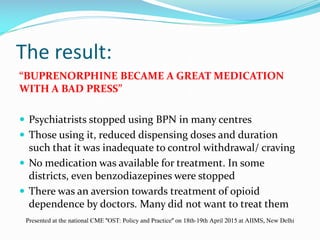
Dr. Ashwin Mohan has been practicing psychiatry since 2001 and treating opioid dependence through opioid substitution therapy (OST) using buprenorphine. He began with a few patients on OST but scaled up treatment in the 2000s as he saw better results than traditional treatment methods. Over the years, he increased doses and duration of OST based on patient needs. However, a 2014 crackdown on opioids led to thousands seeking treatment without adequate infrastructure. This created diversion issues and negative press around OST. As a result, many psychiatrists stopped OST and treatment options were severely limited, worsening the opioid crisis. Dr. Mohan argues for expanding access to OST and other evidence-based treatments for opioid dependence.