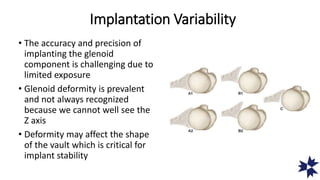
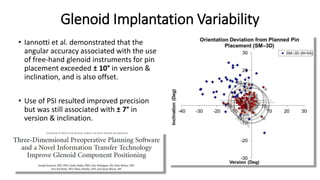
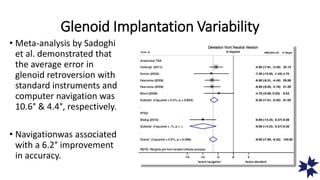
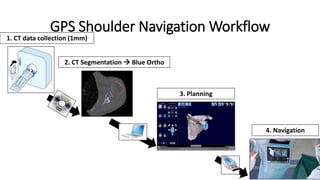
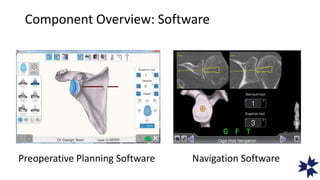
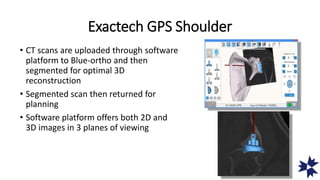
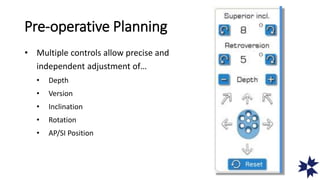
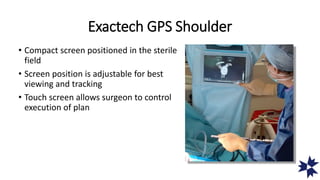
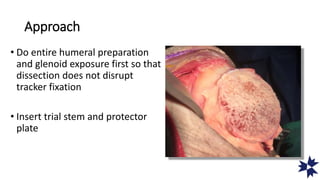
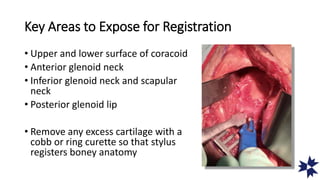
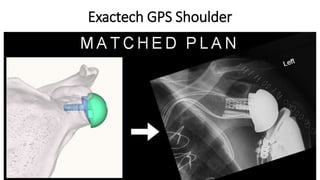
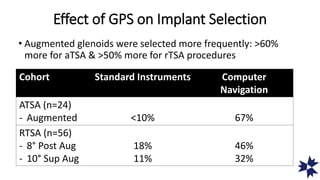
The document discusses the challenges and advancements in glenoid component implantation in shoulder arthroplasty, highlighting issues such as glenoid deformity and the impact of retroversion on implant stability. It emphasizes the importance of accurate preoperative planning and navigation technology, like Exactech GPS, which enhances precision in implant placement. The use of advanced imaging and navigation techniques is presented as a means to improve surgical outcomes and reduce variability in implant positioning.