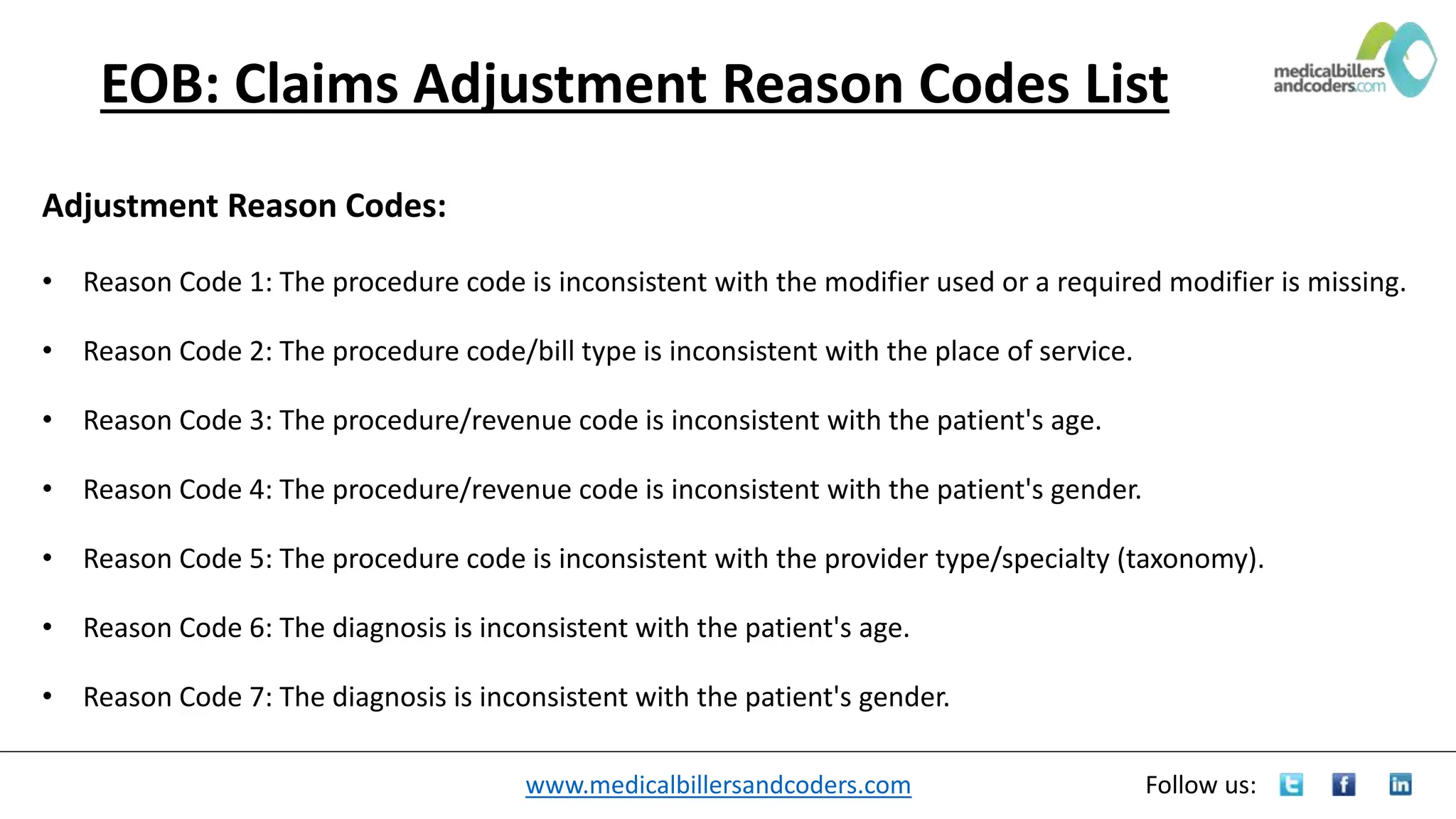
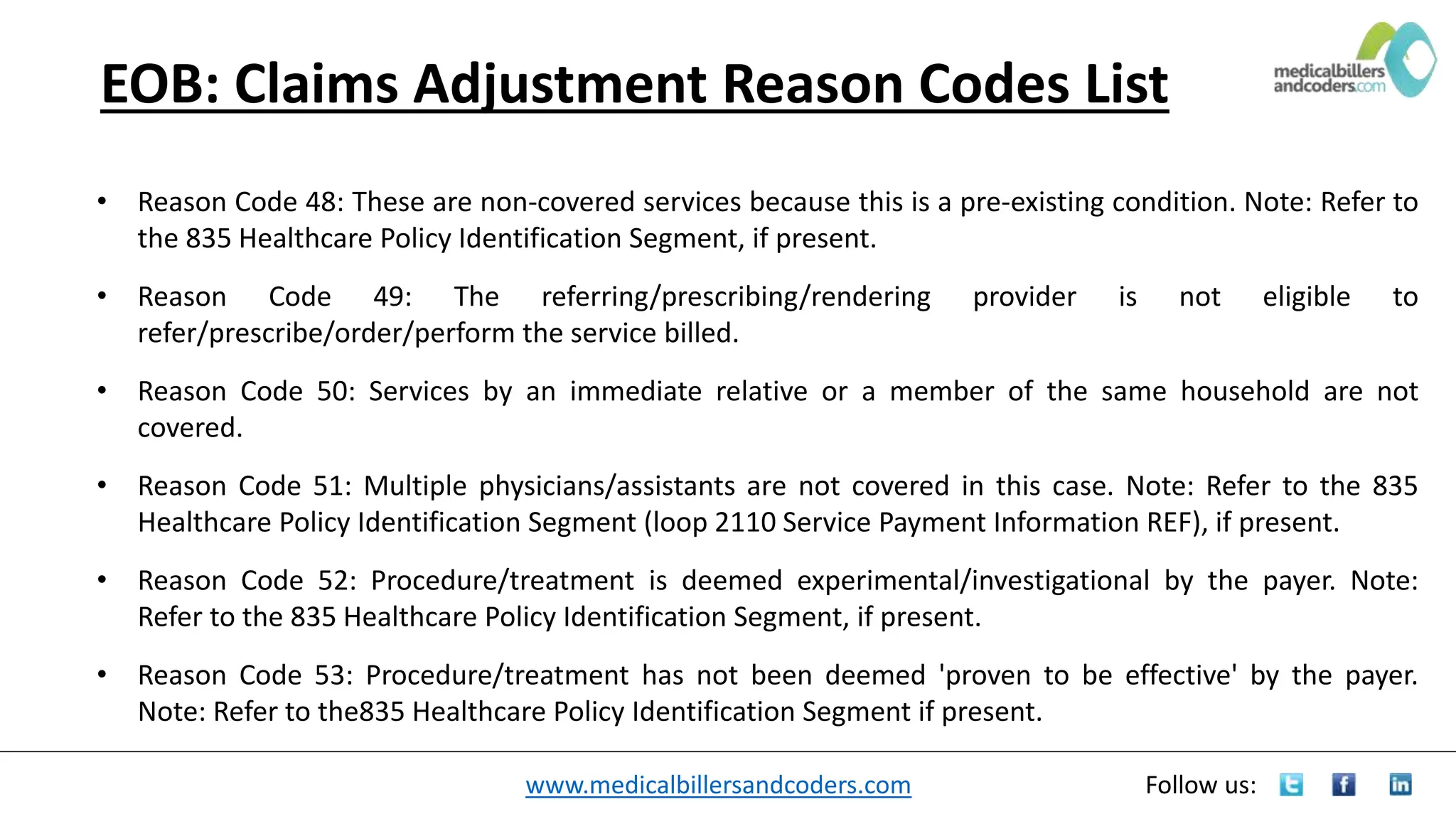
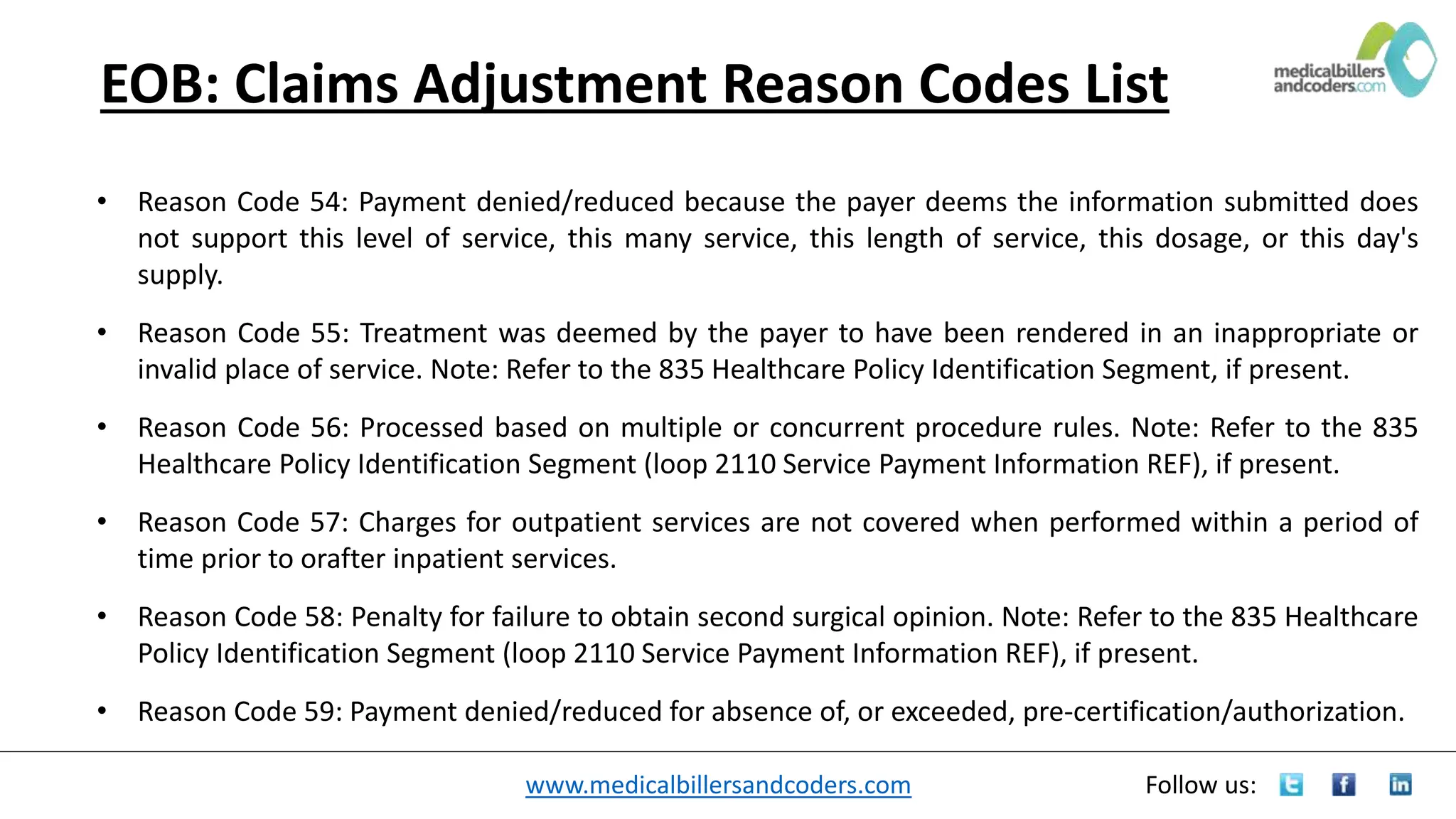
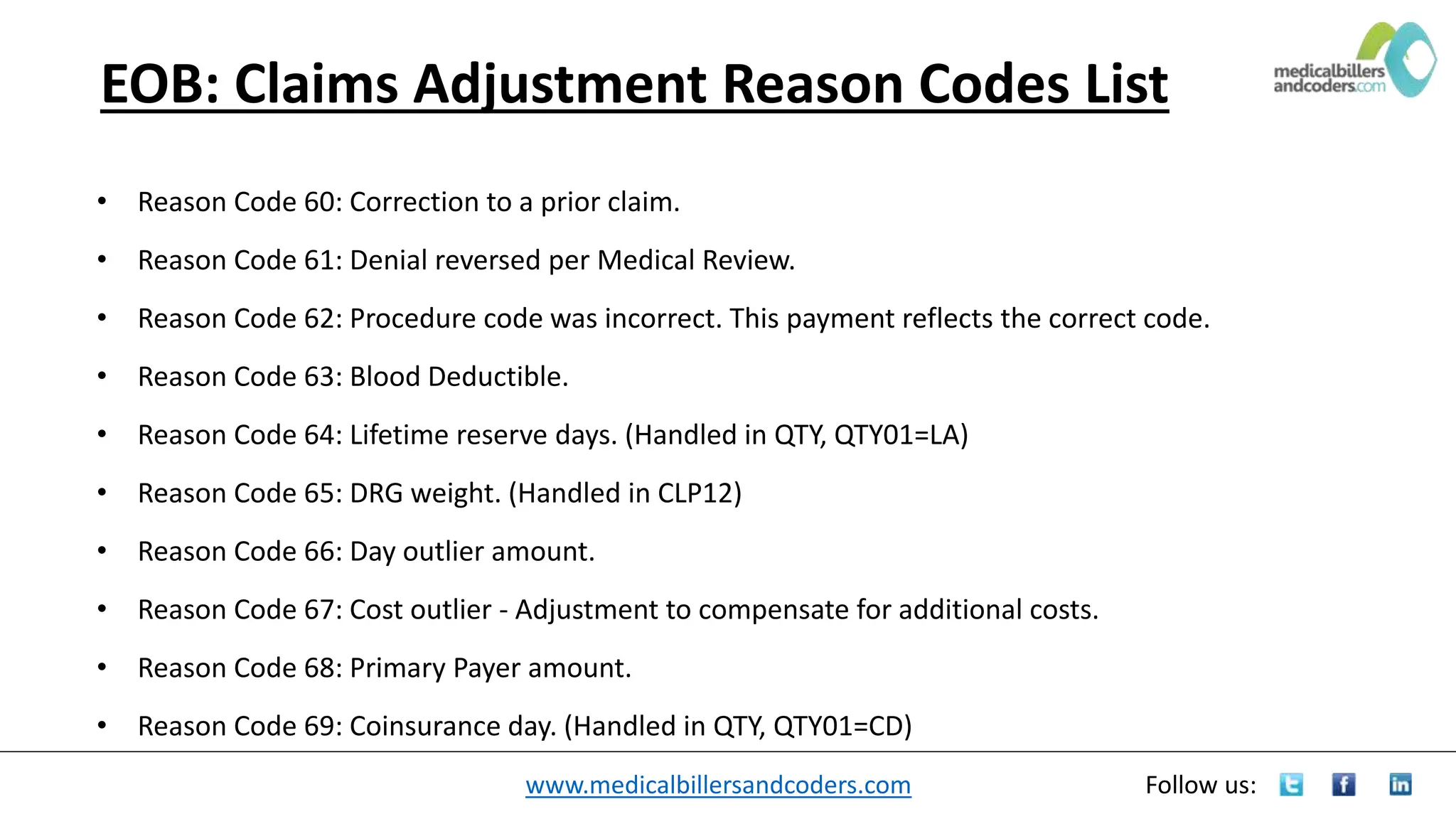
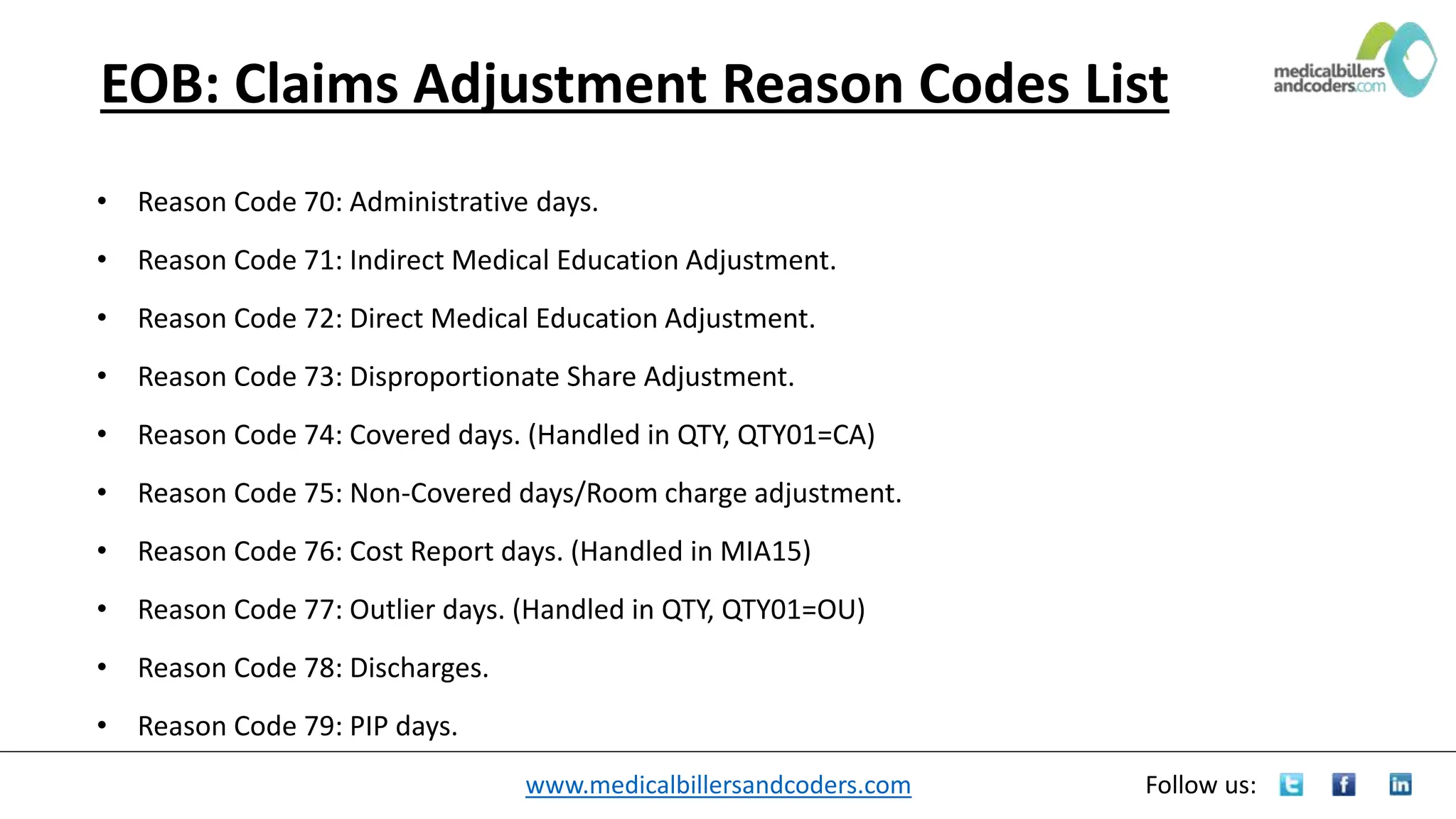
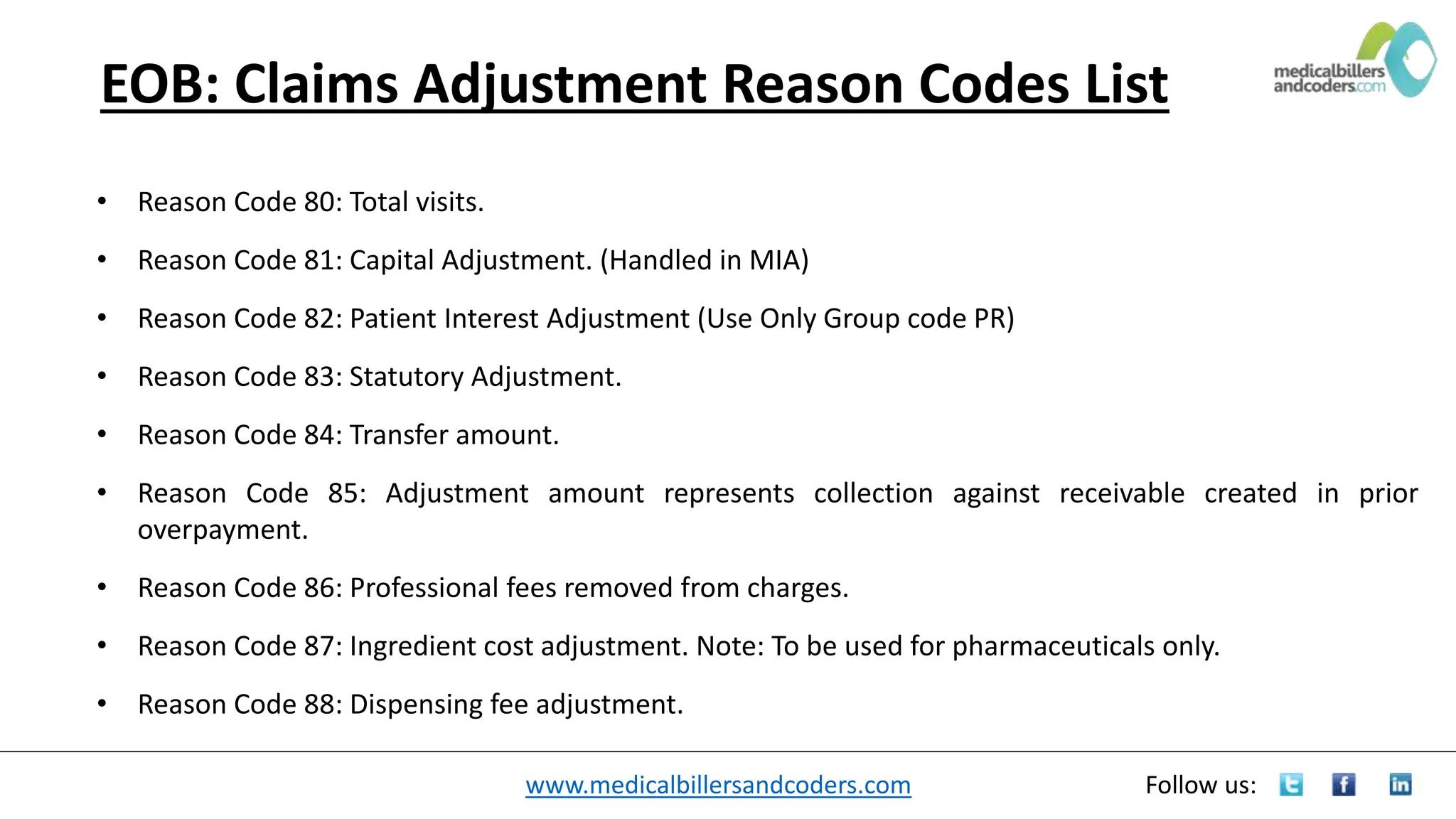
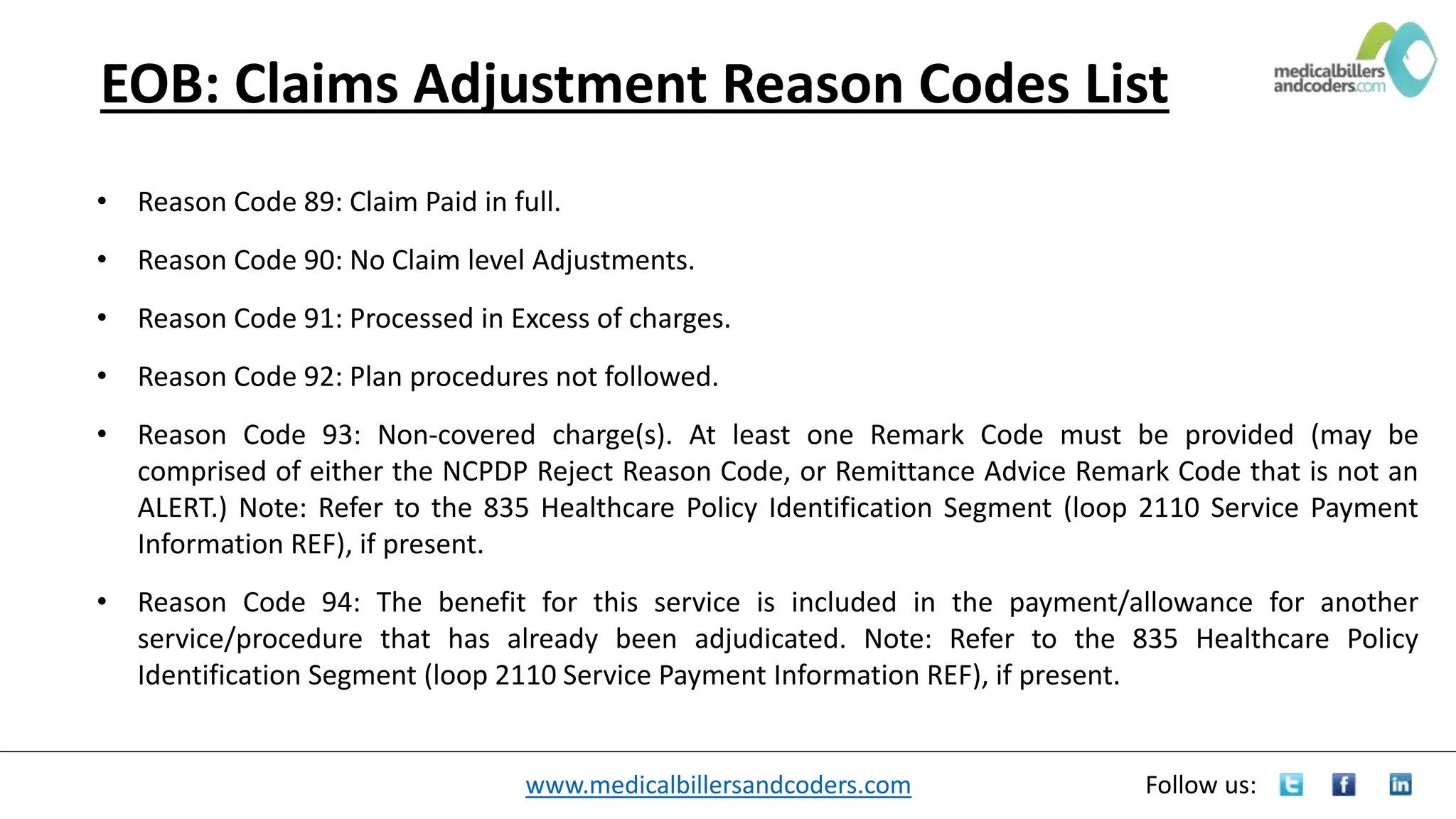
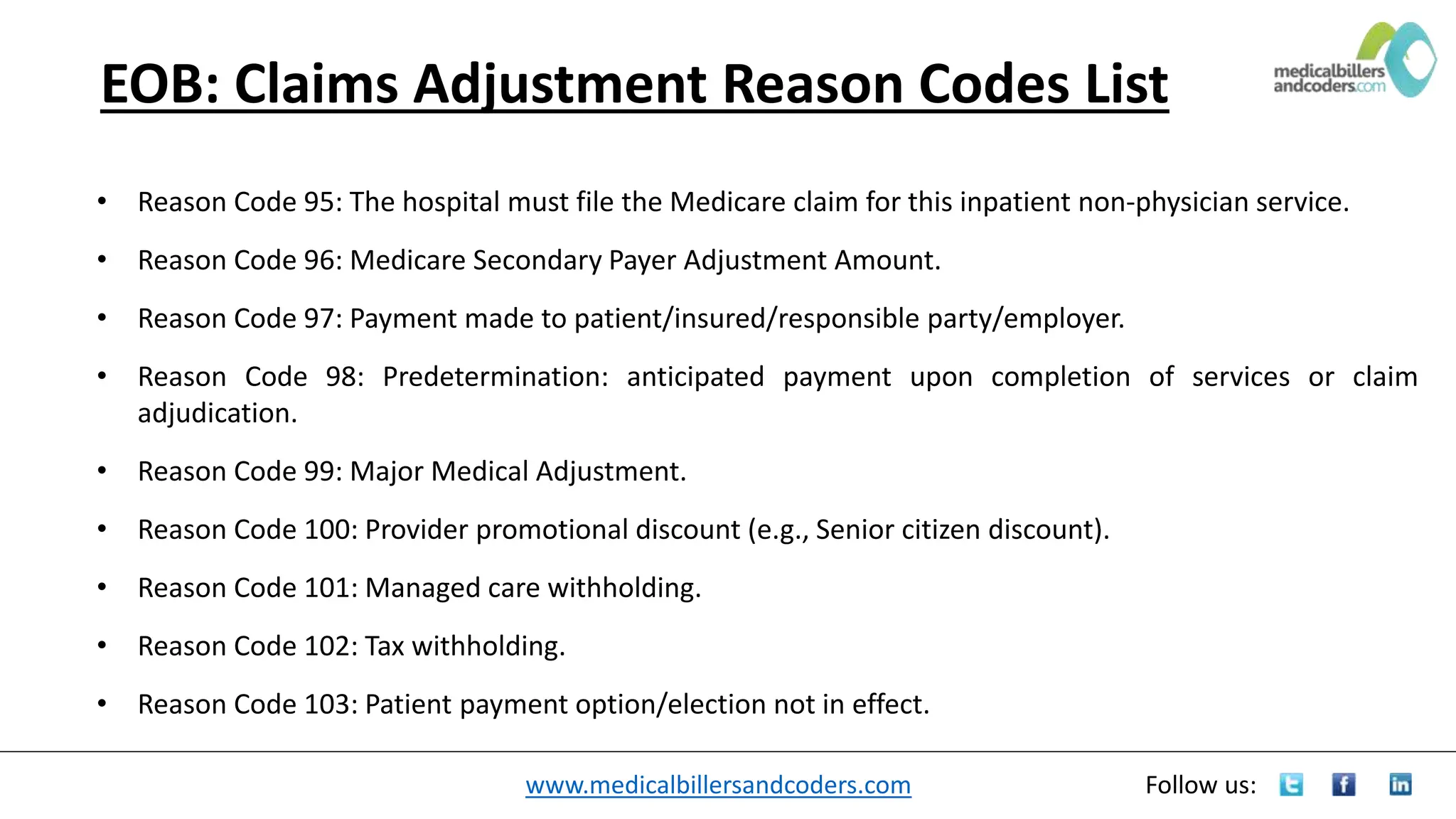
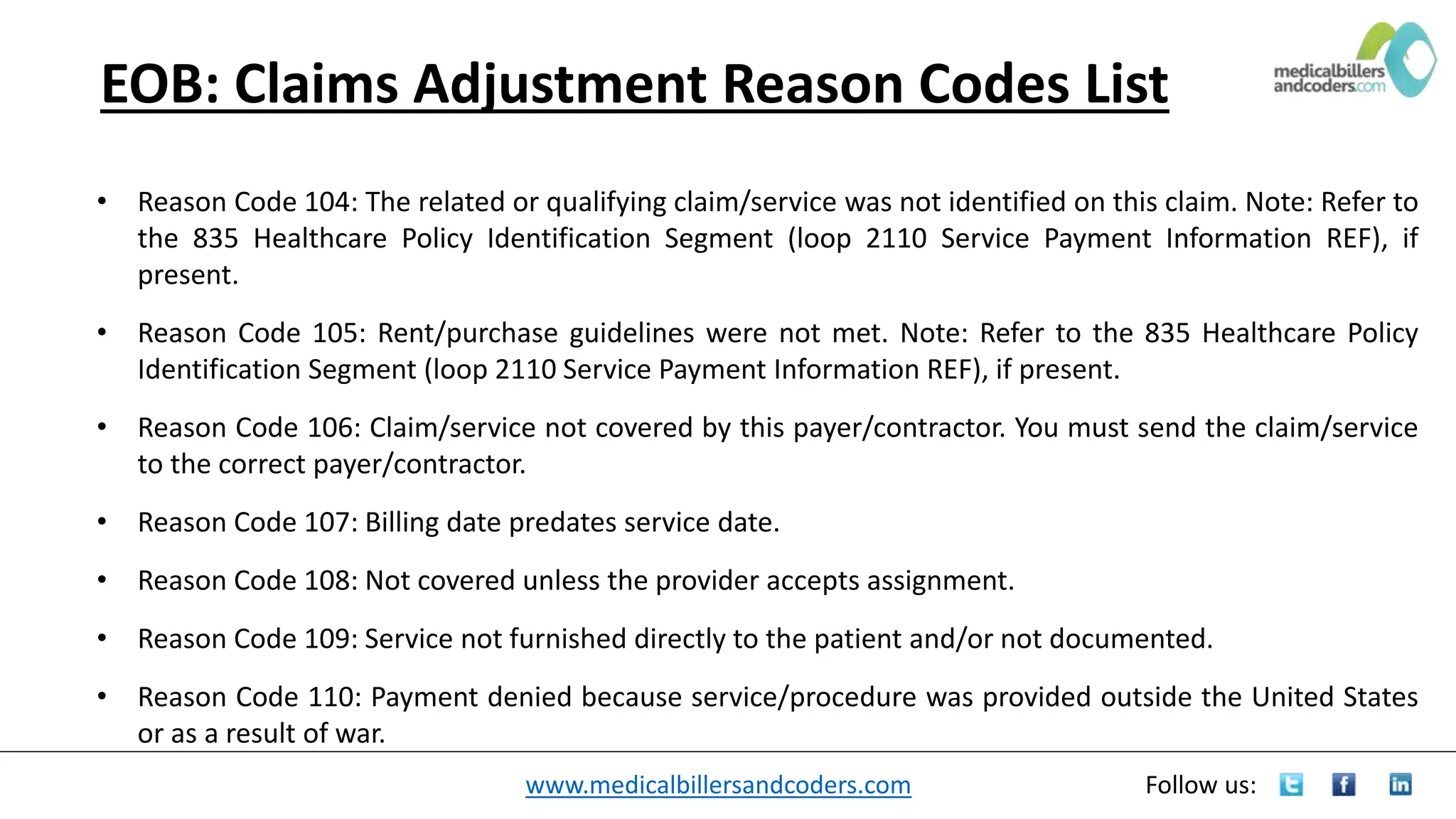
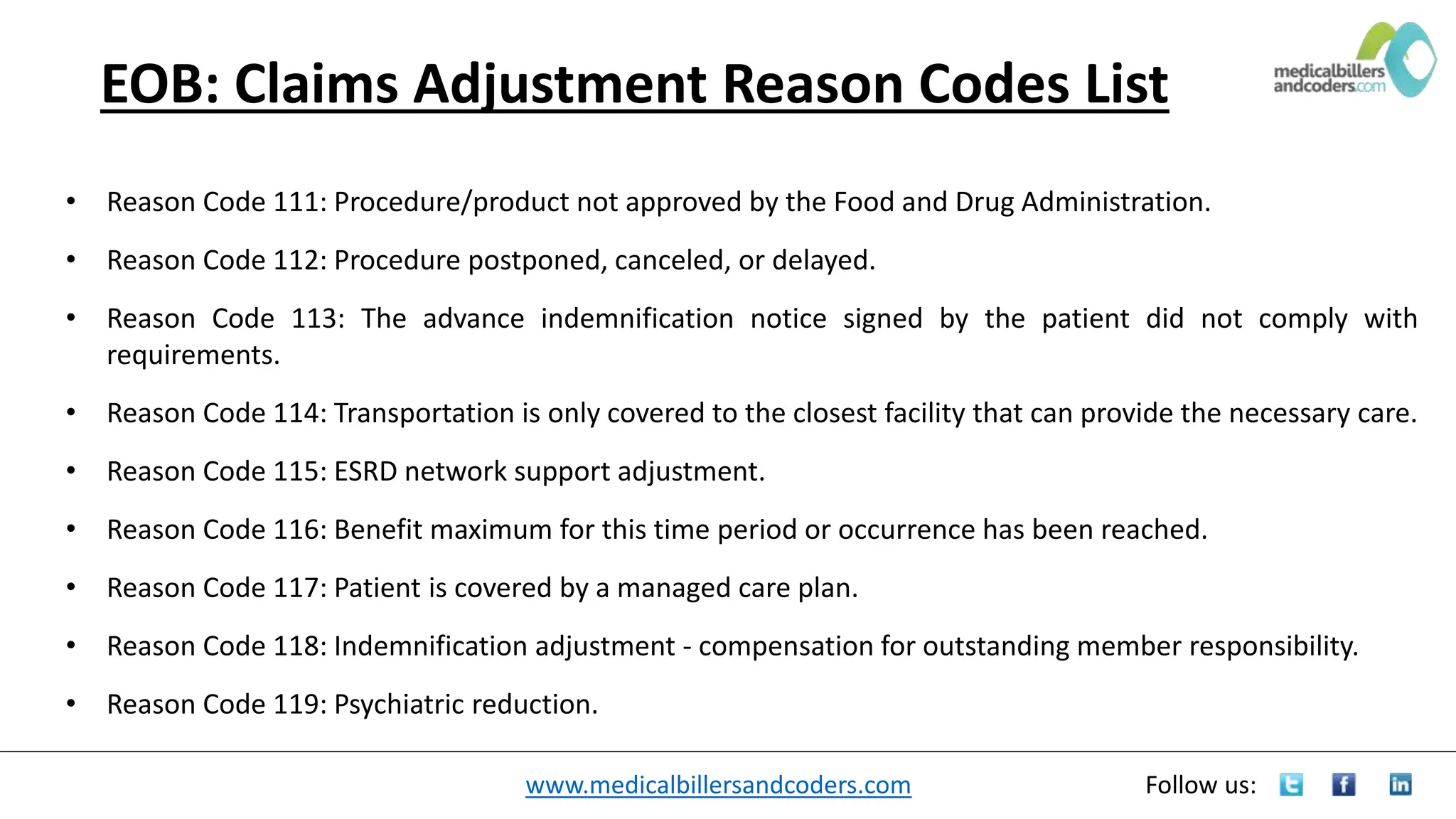
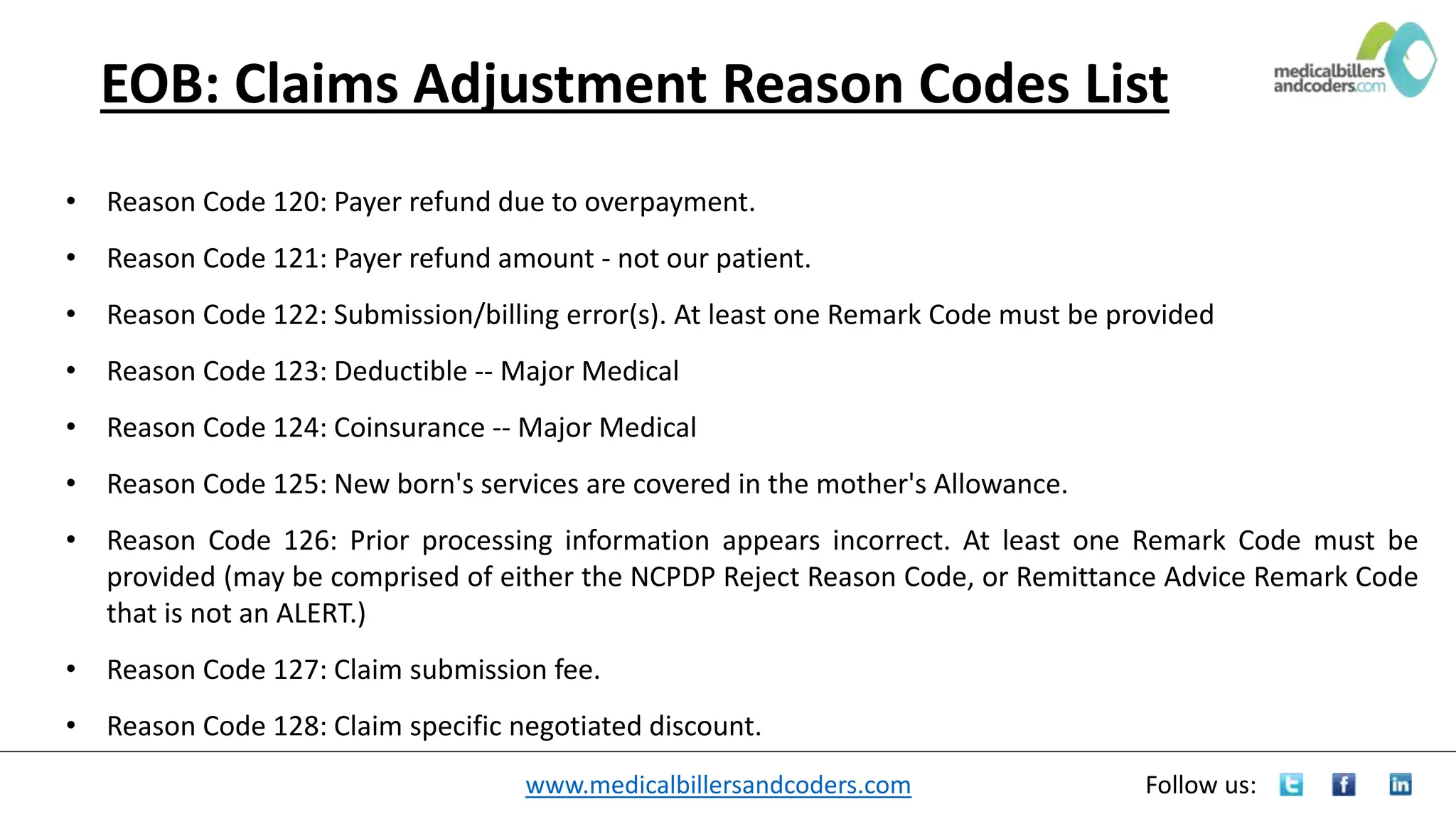
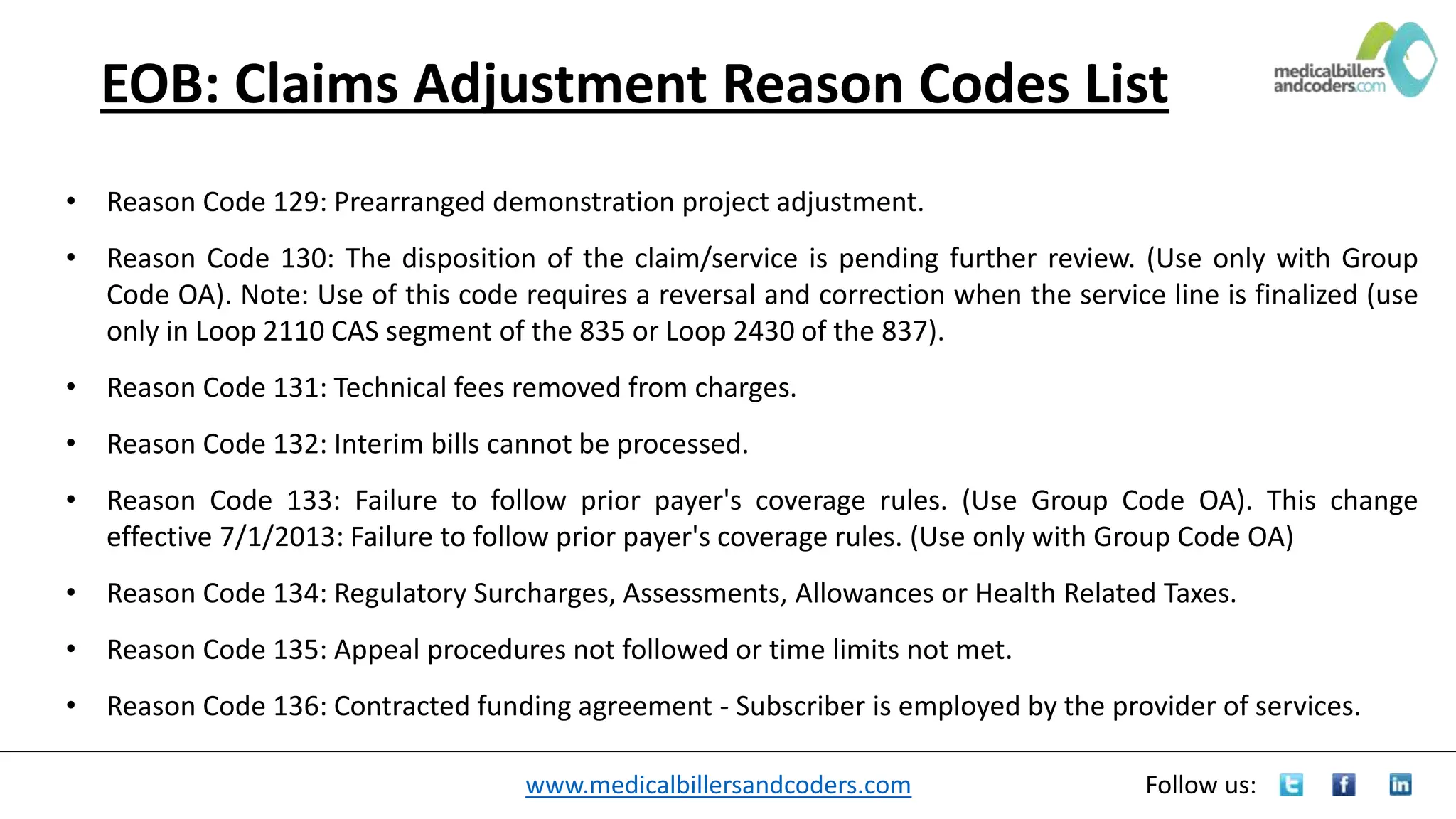
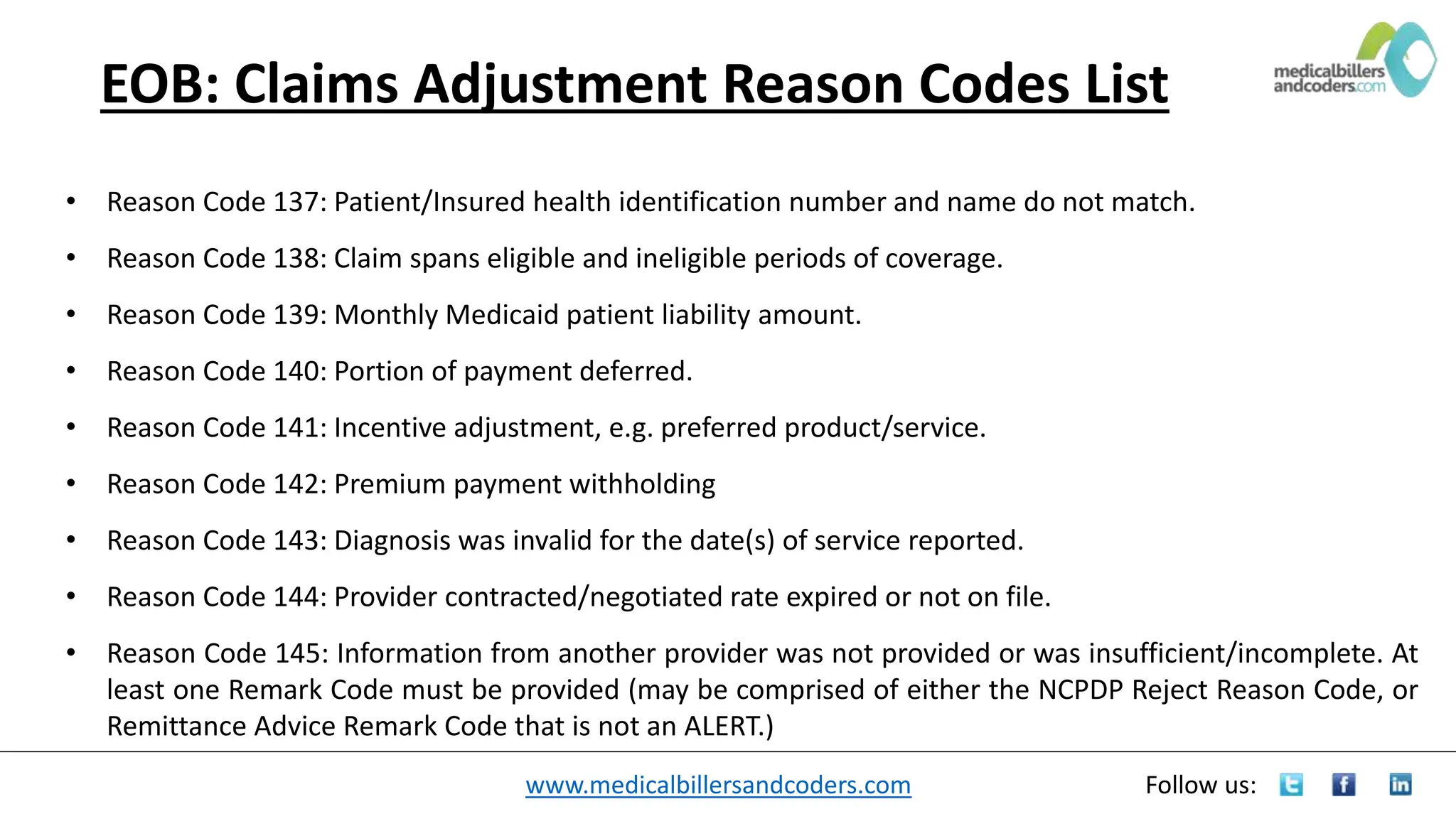
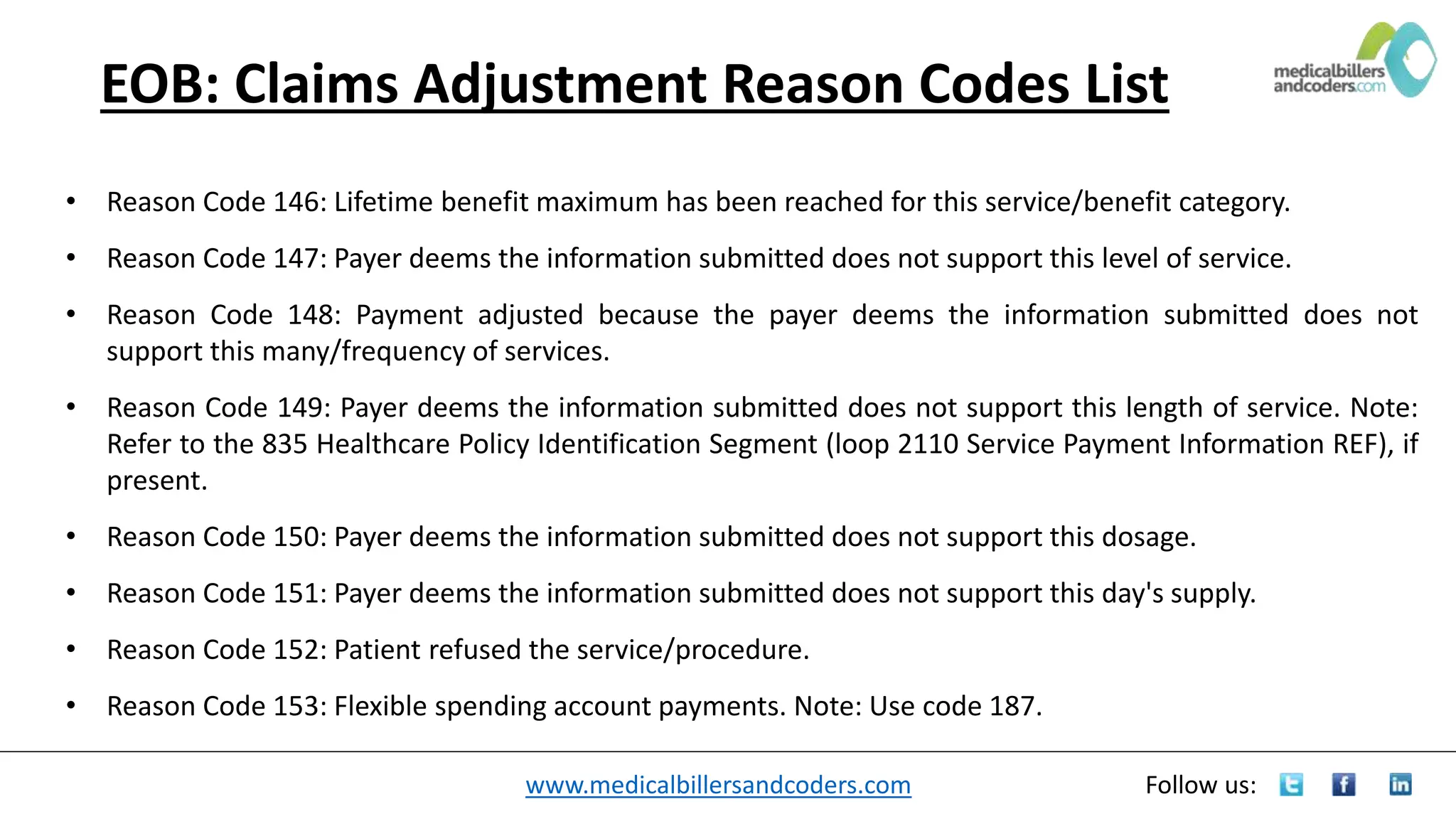
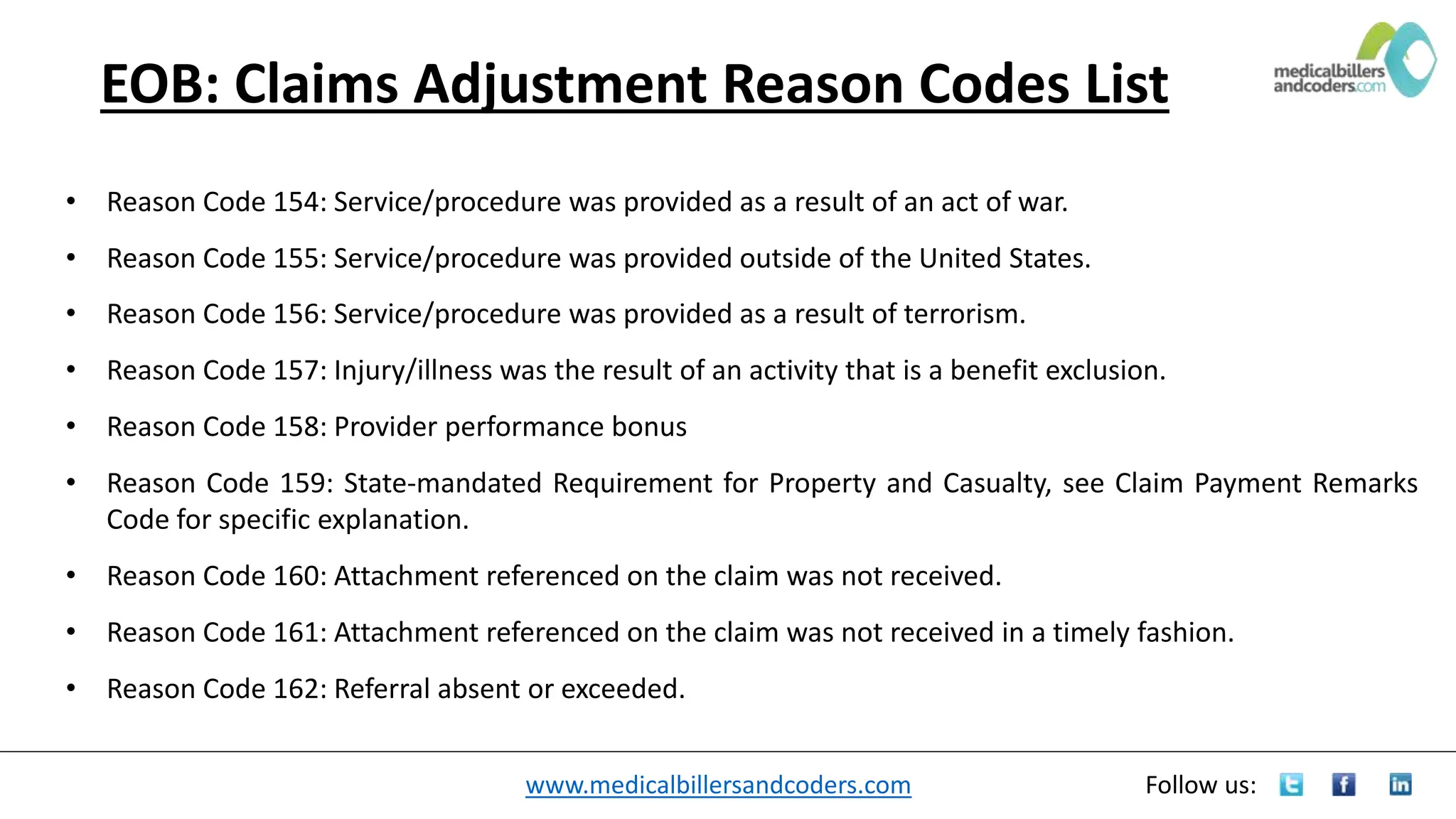
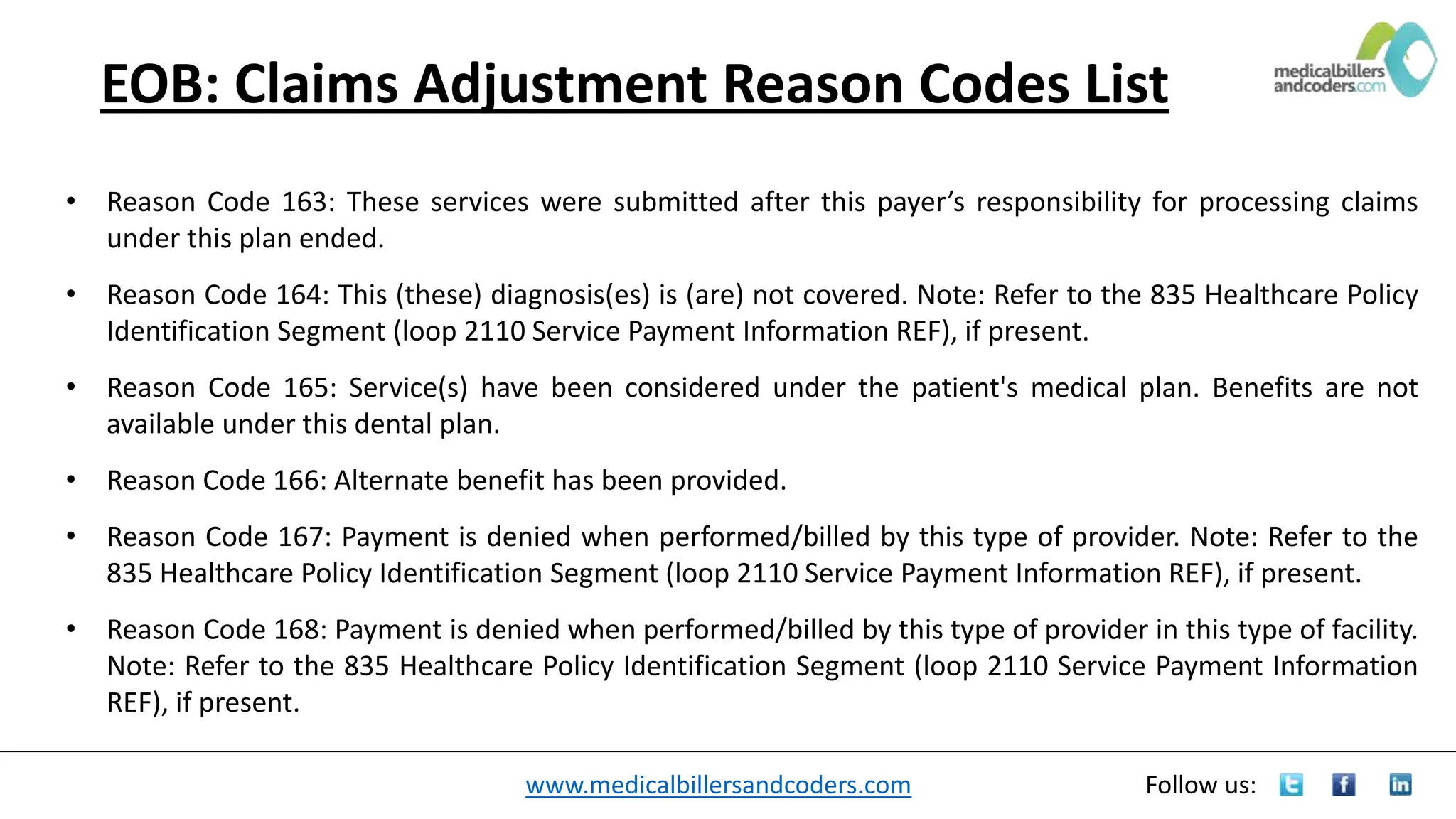
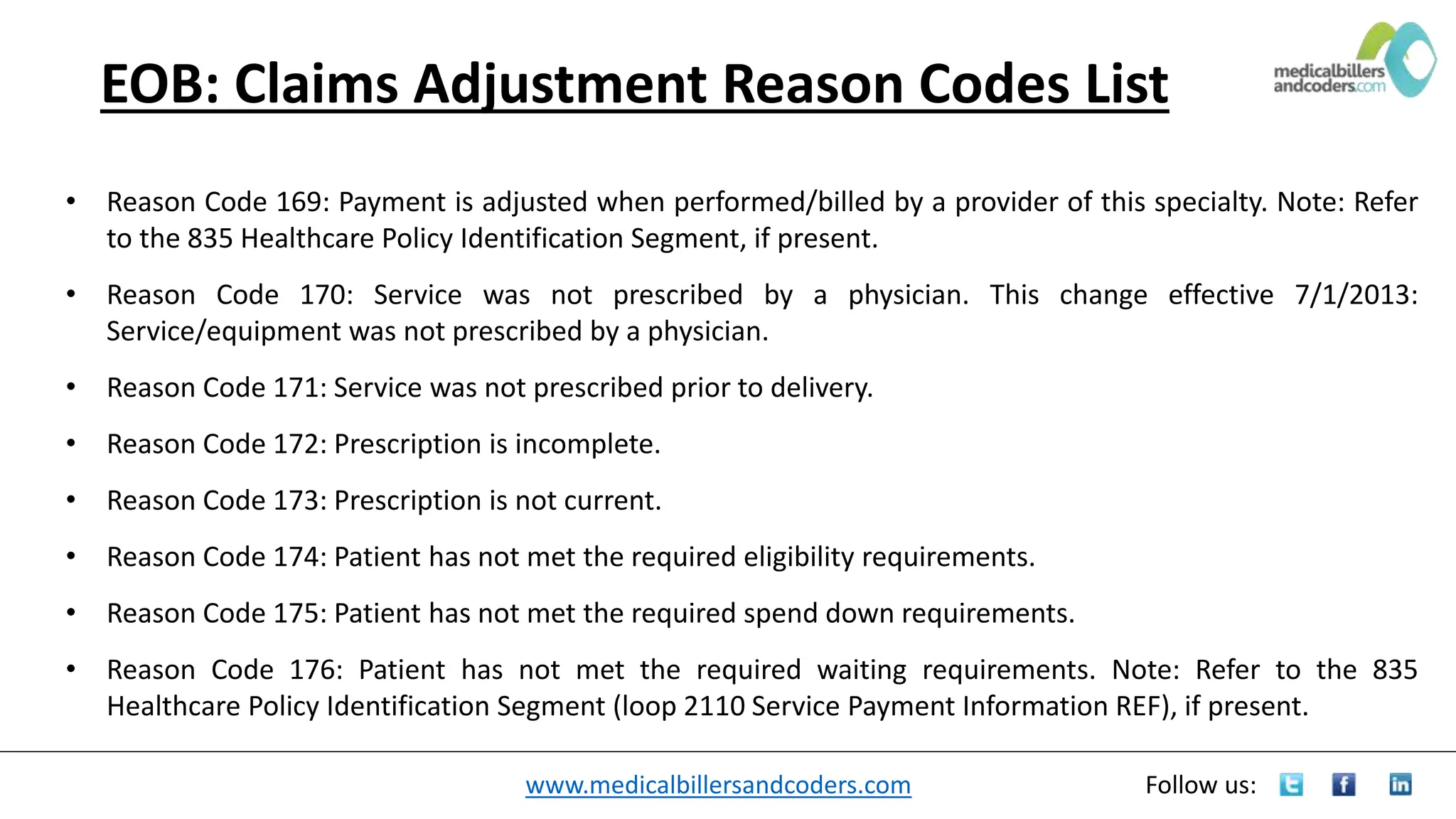
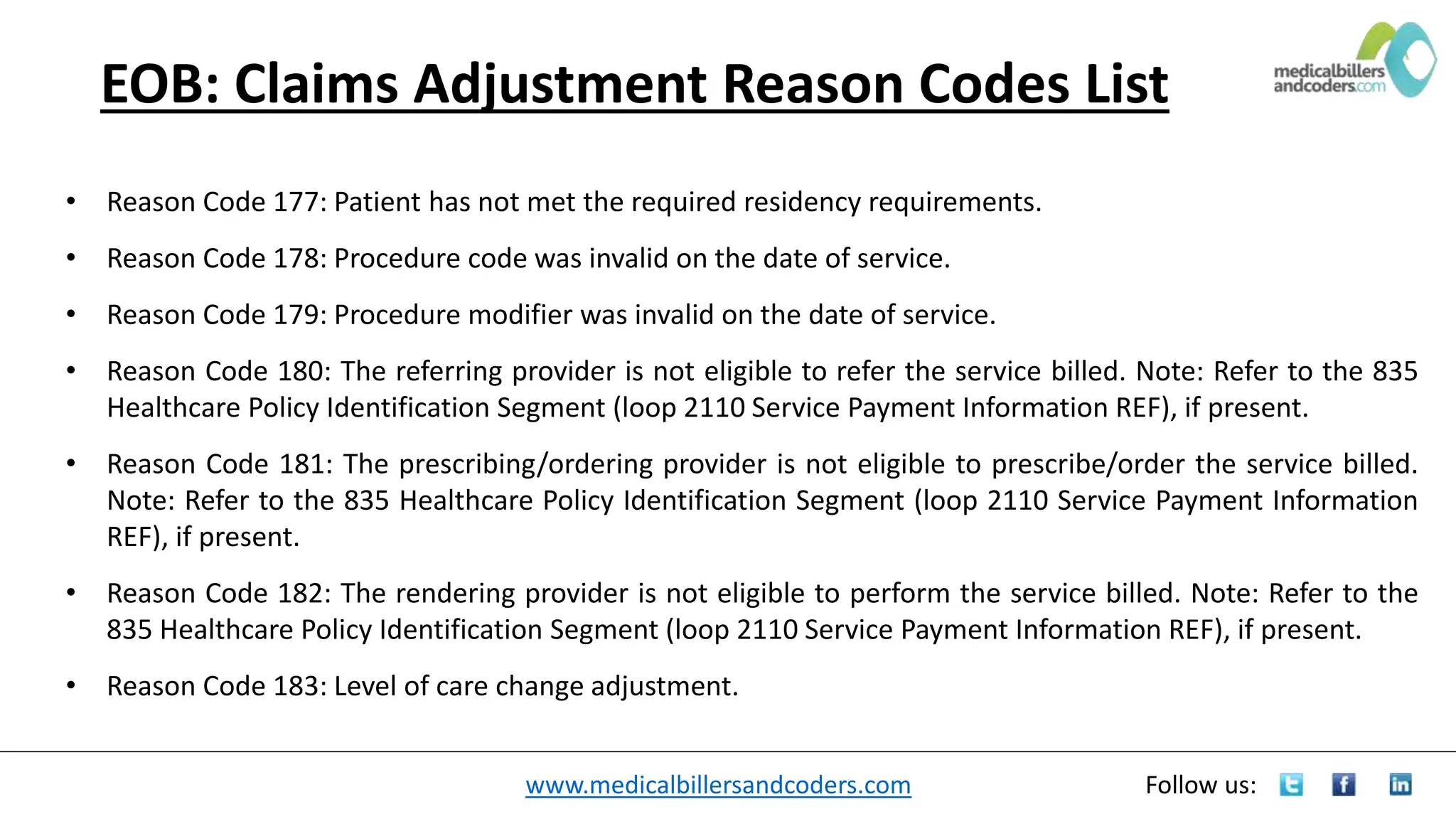
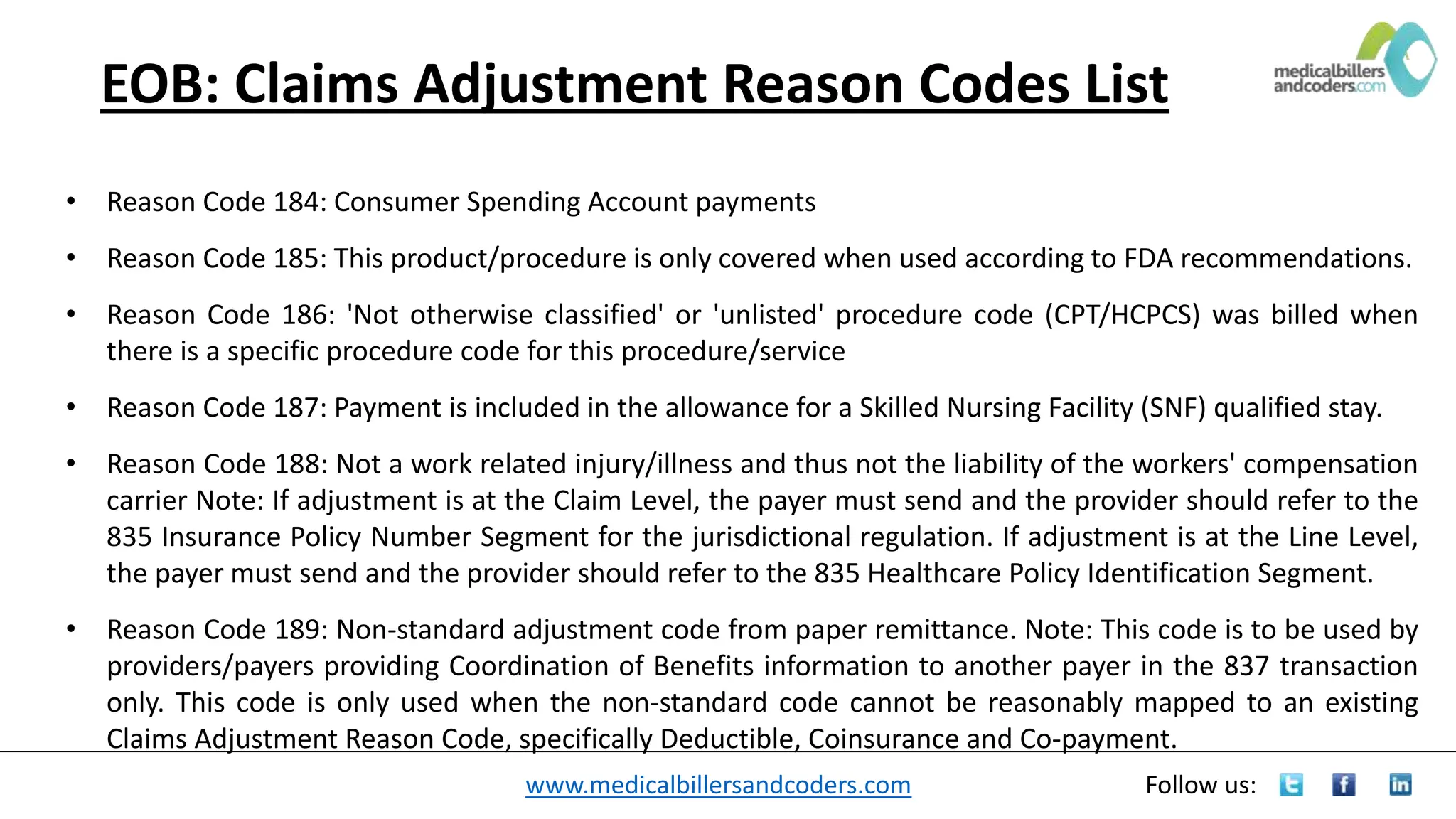
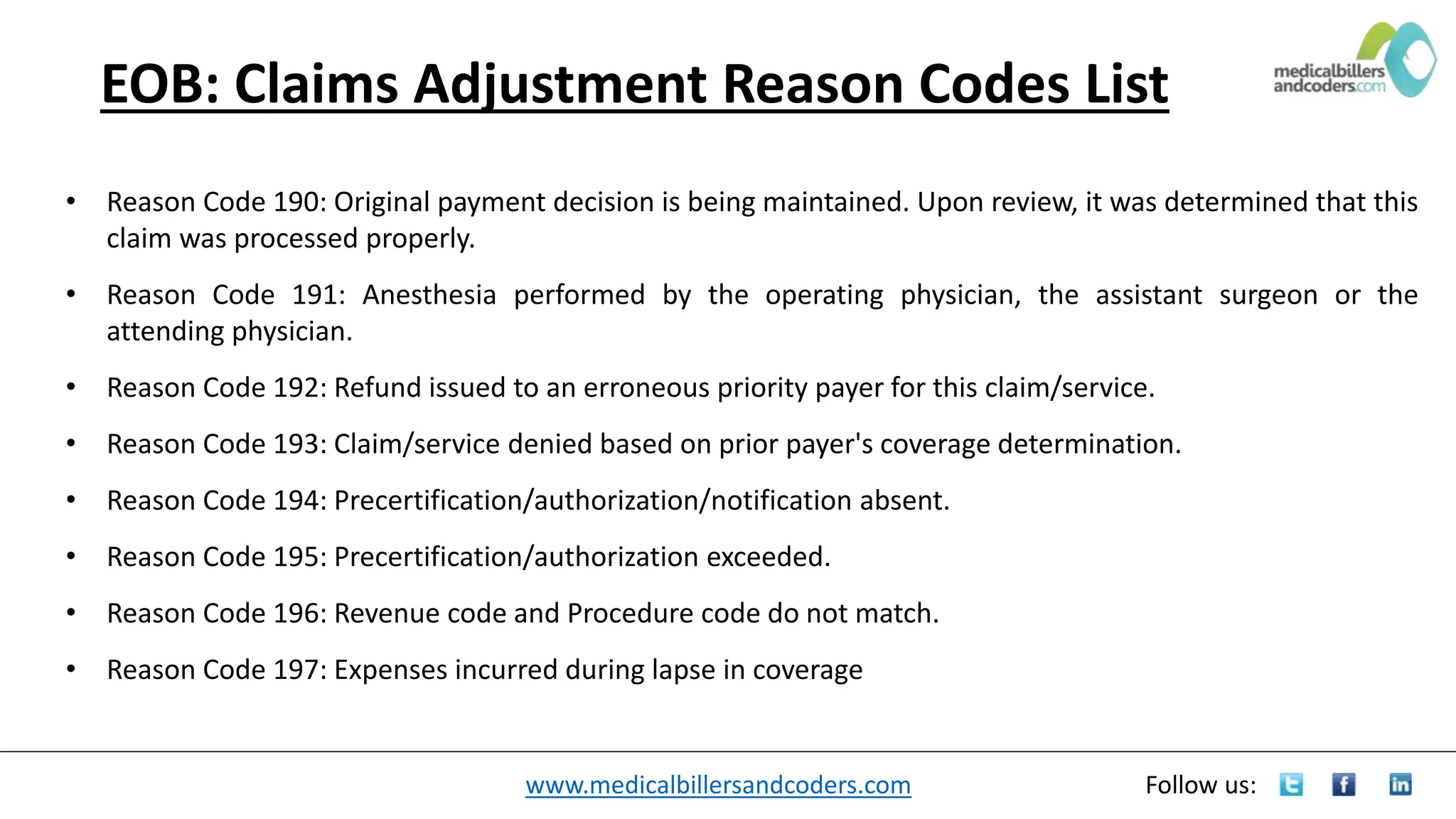
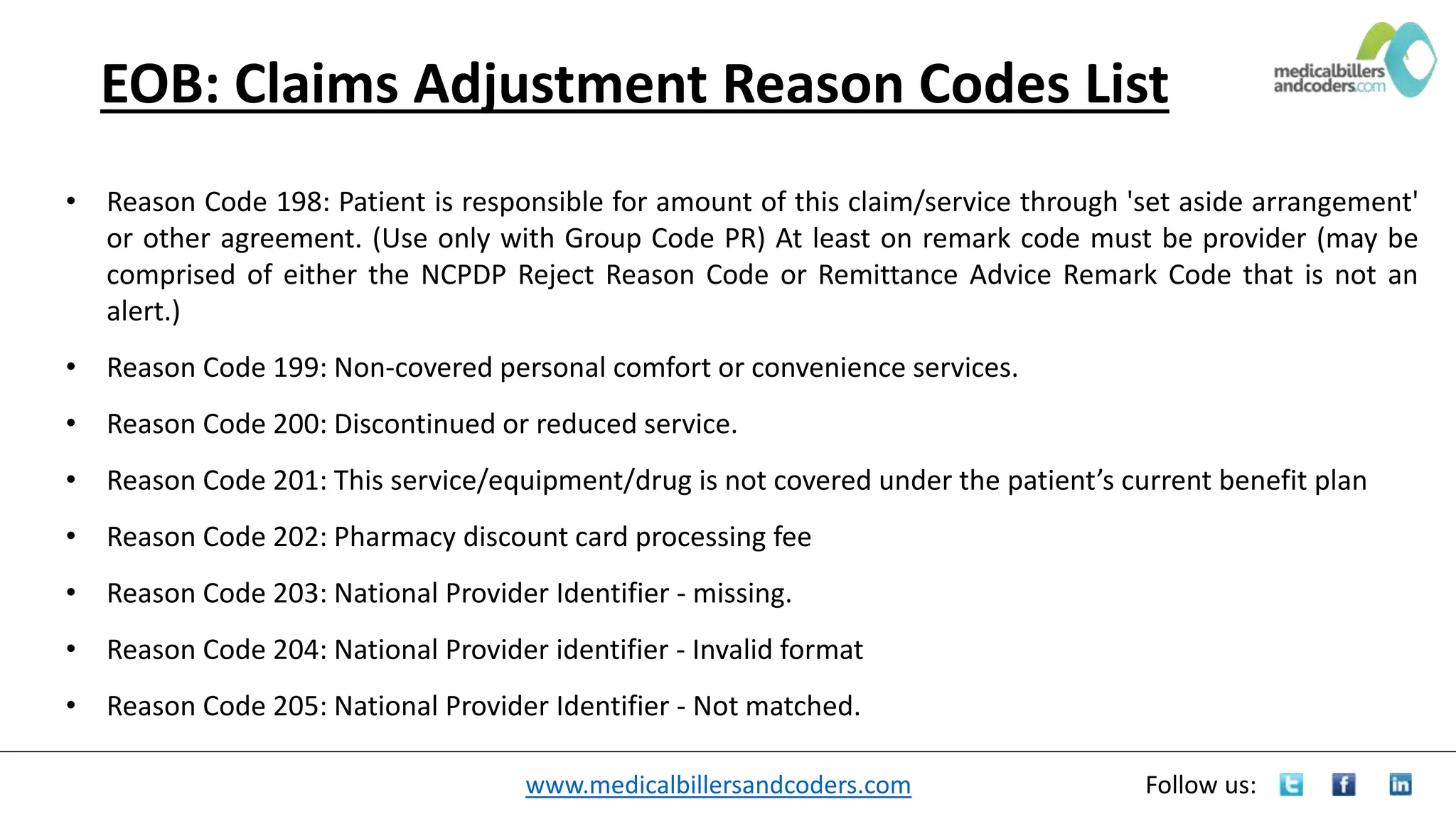
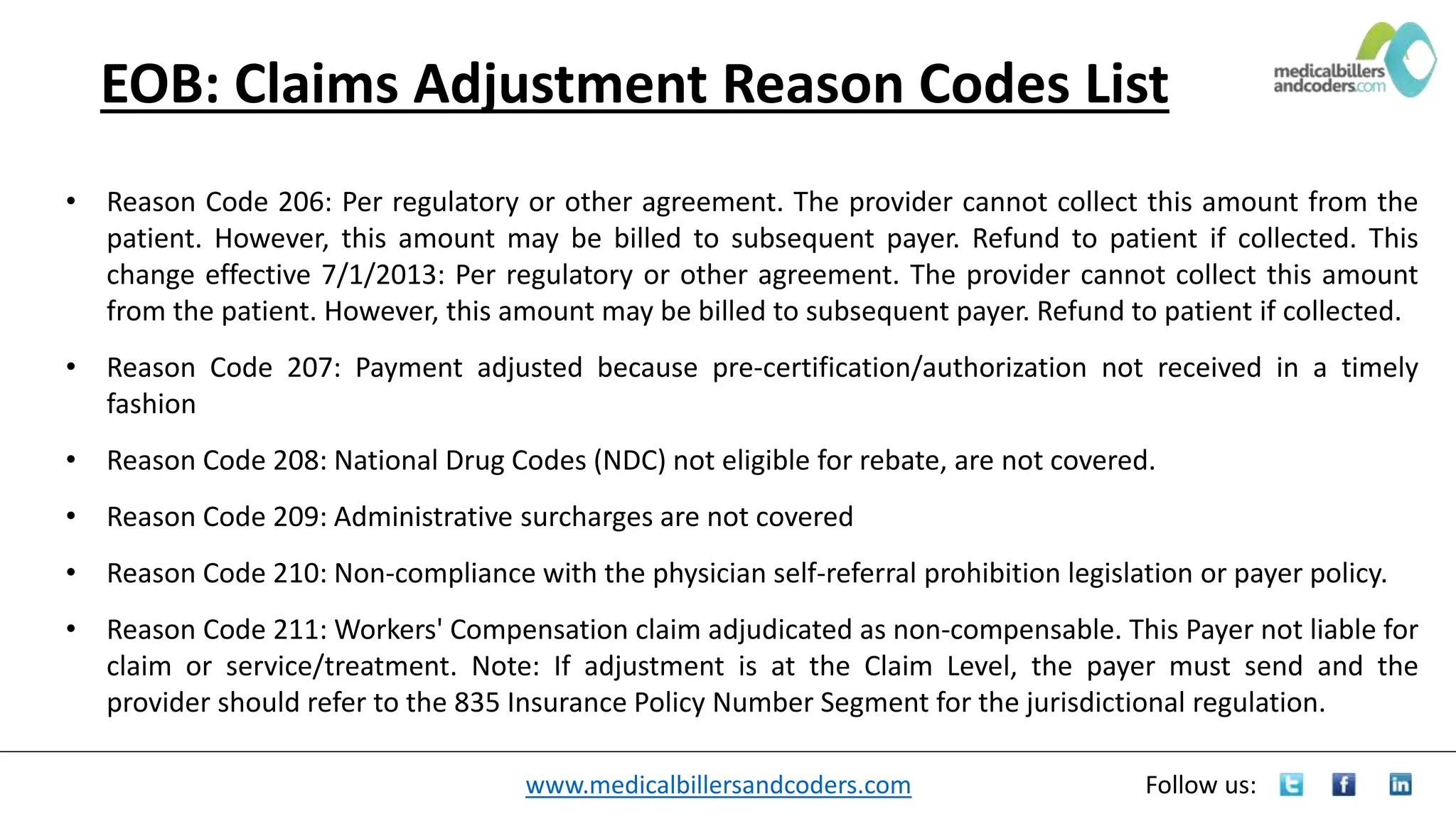
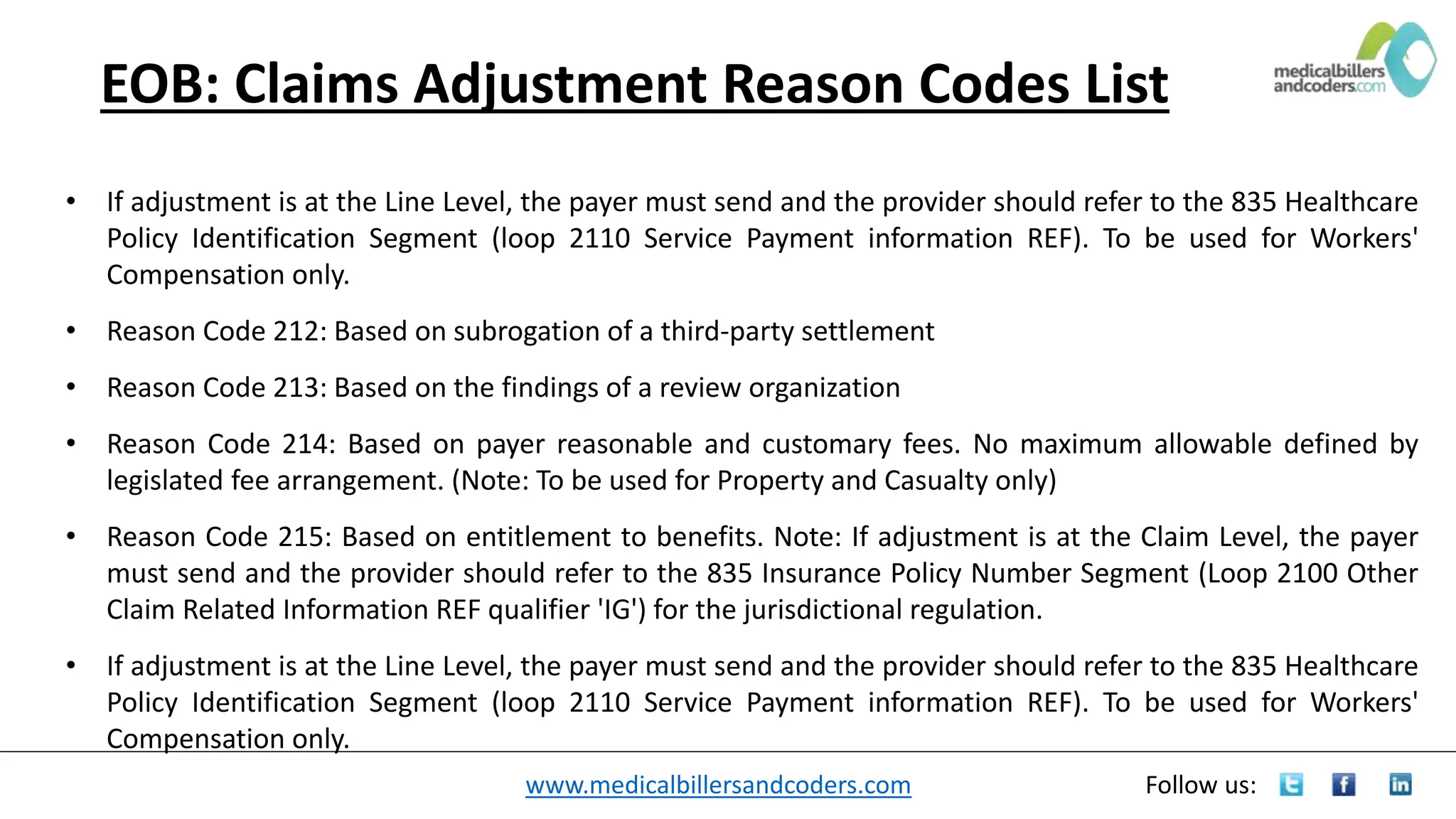
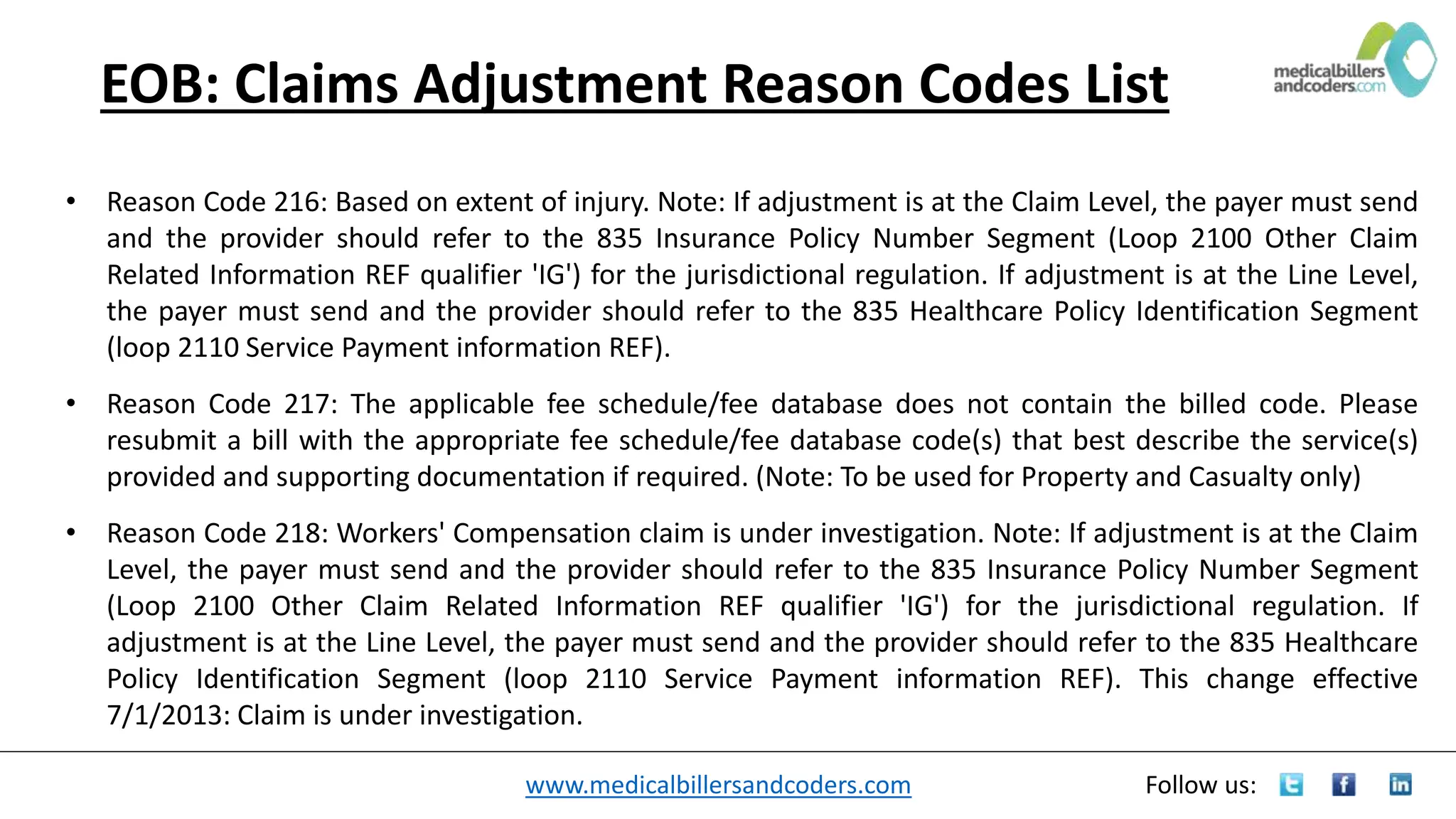
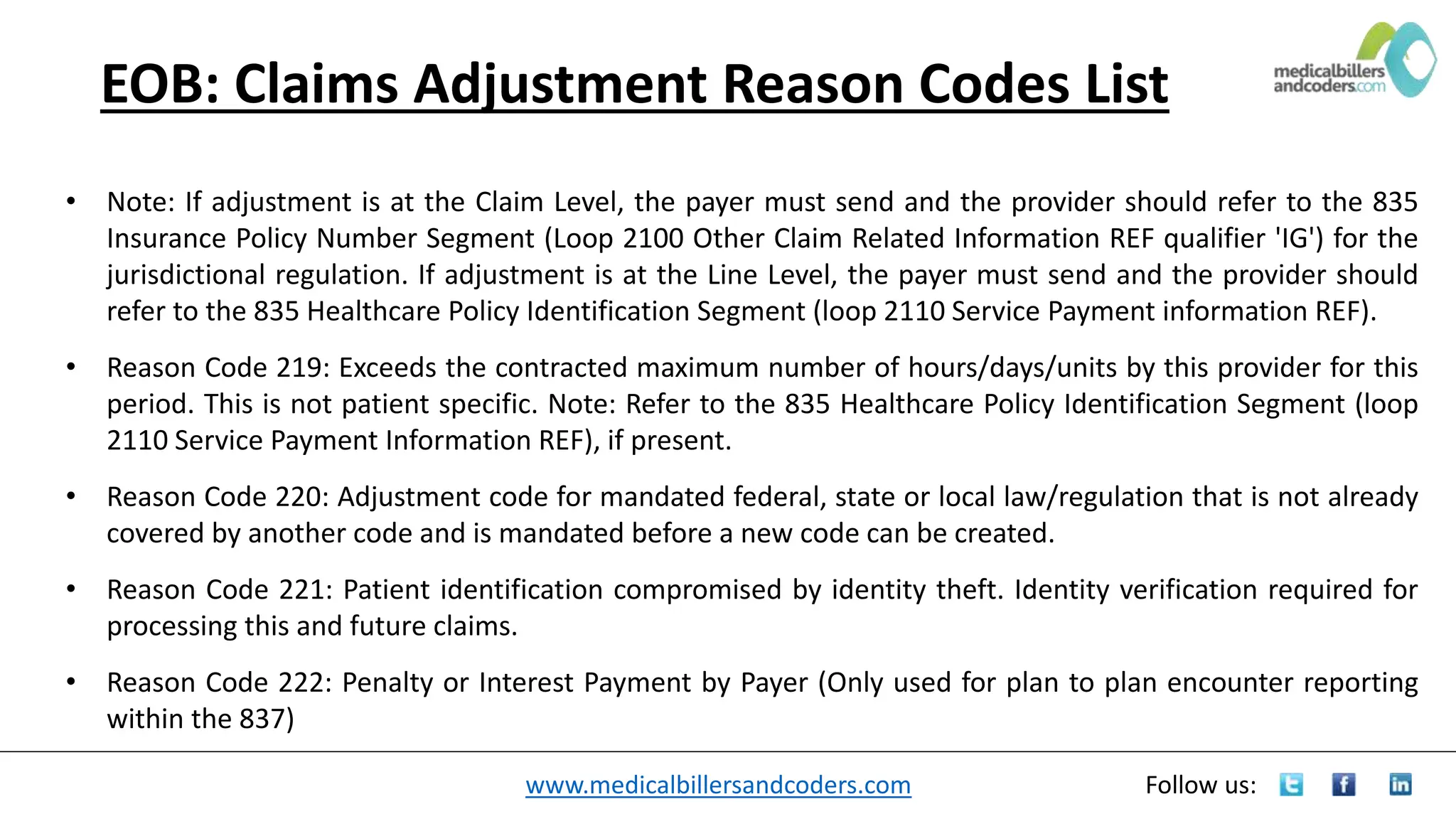
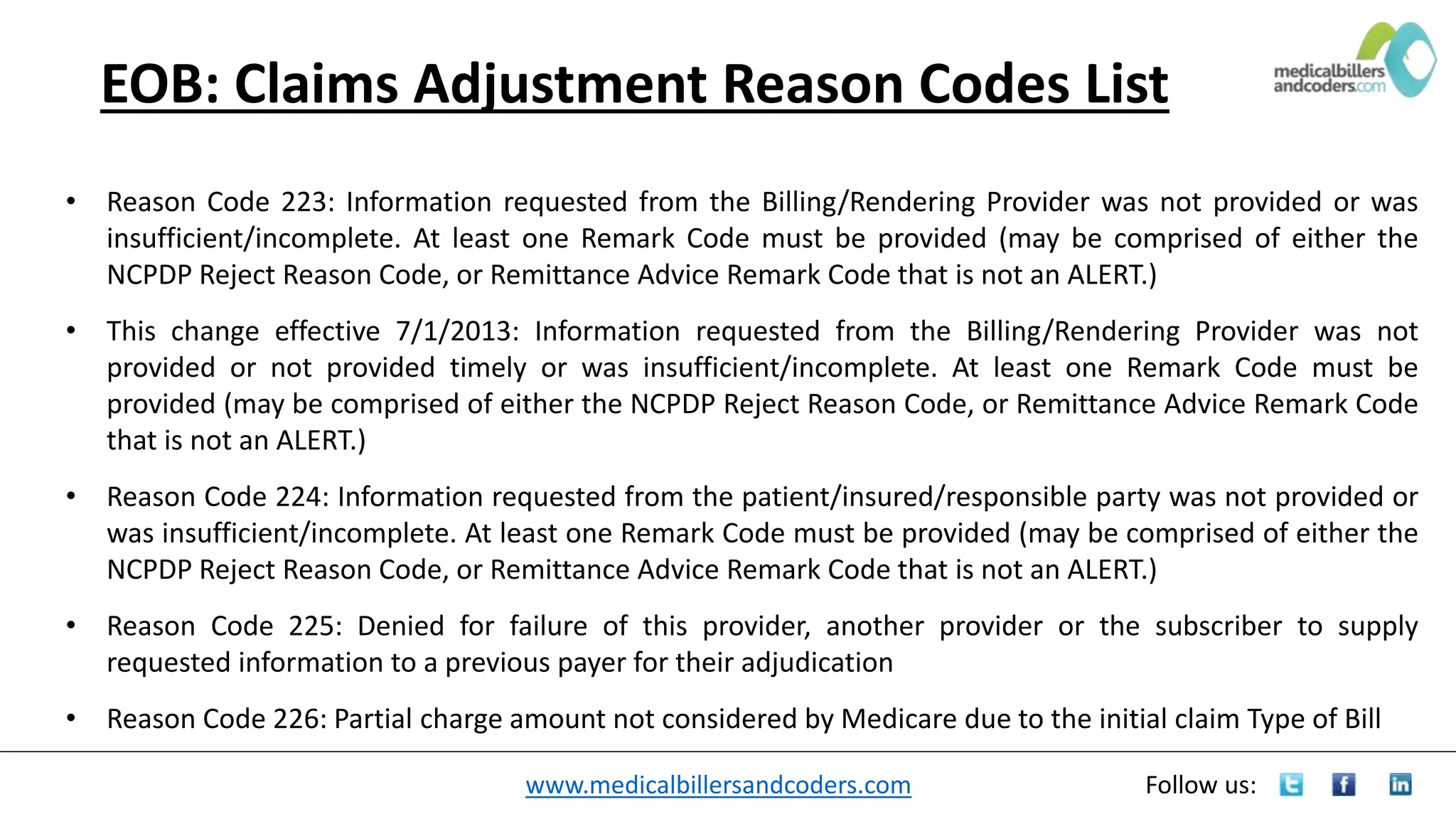
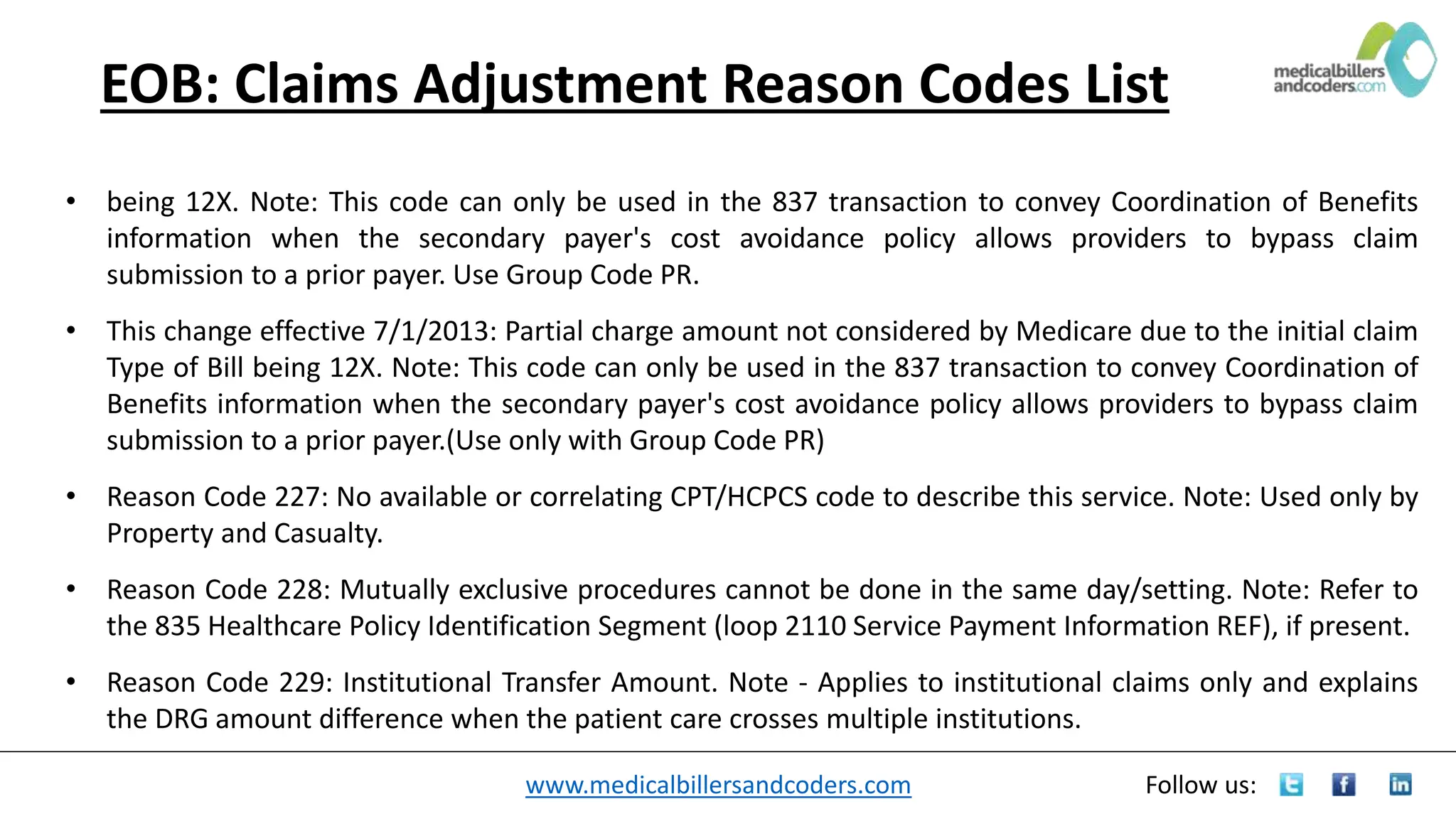
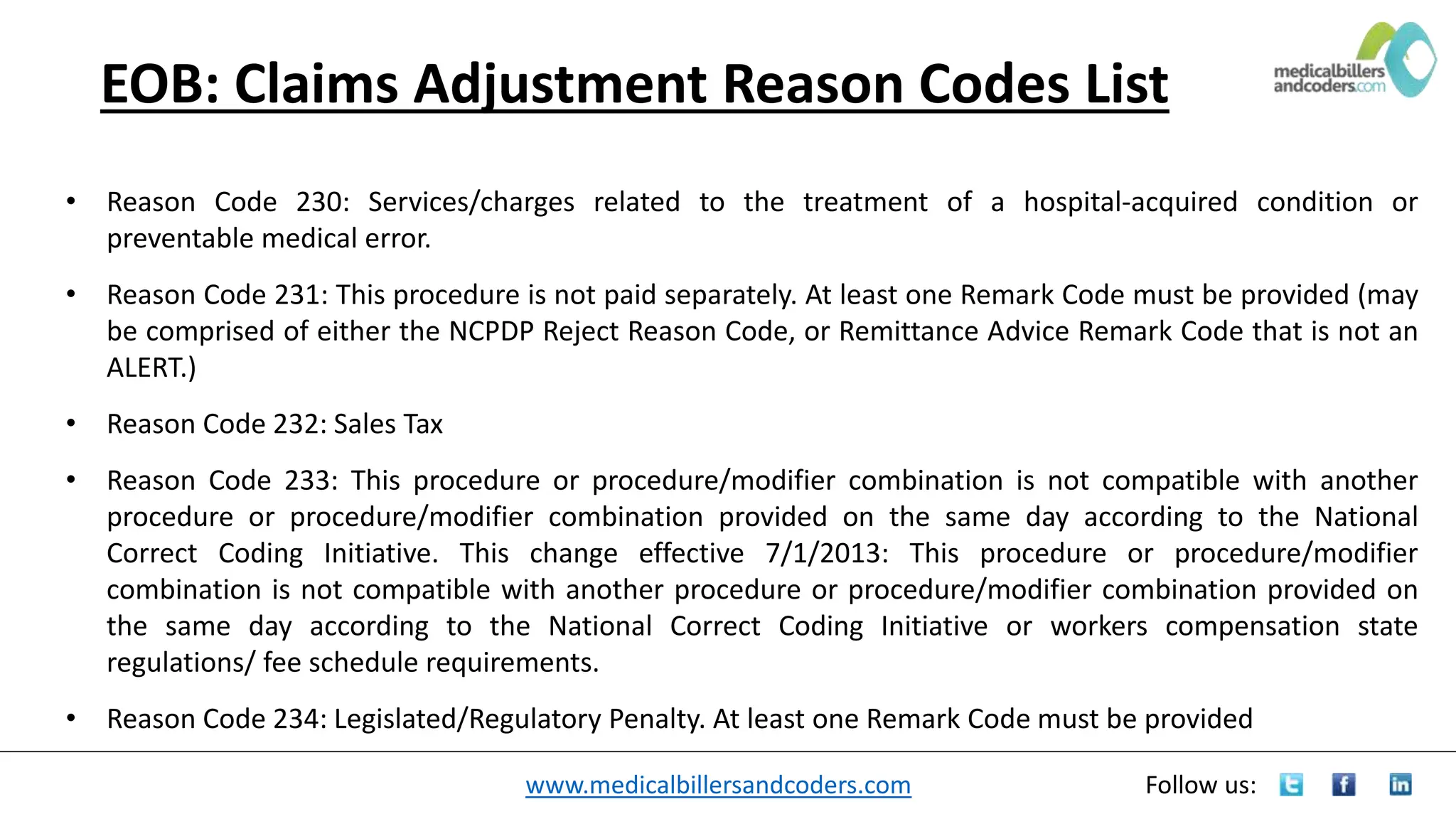
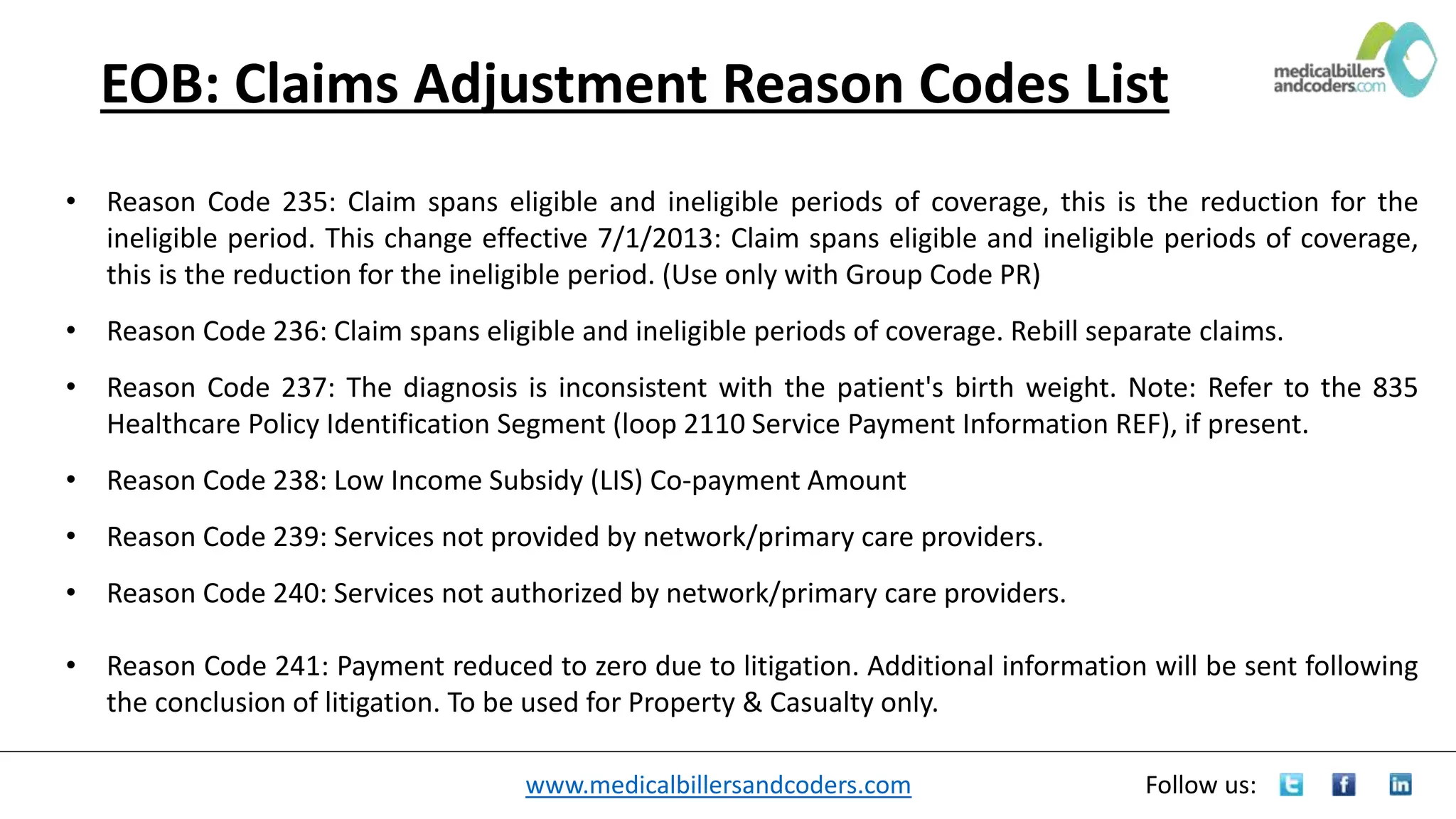
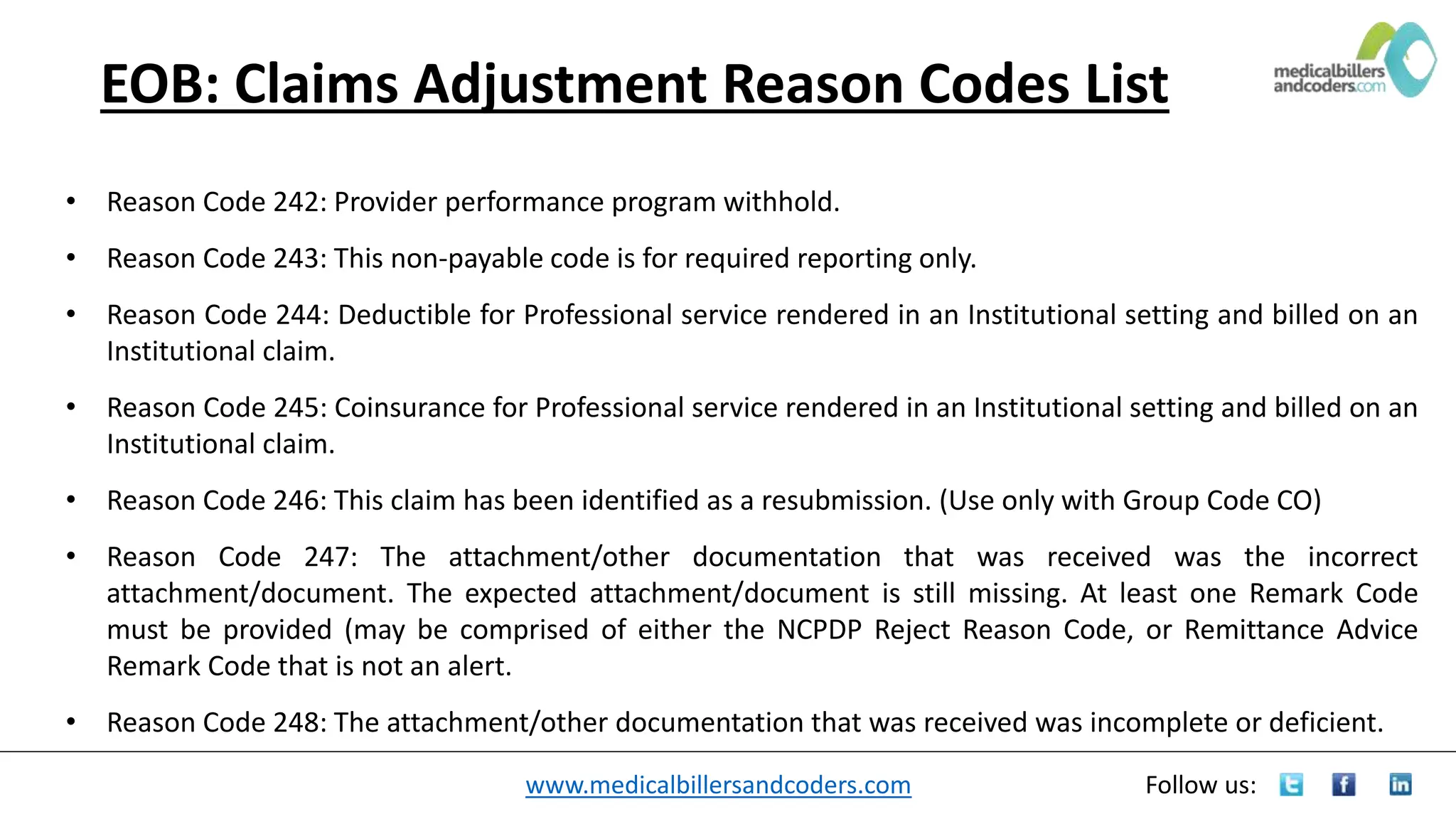
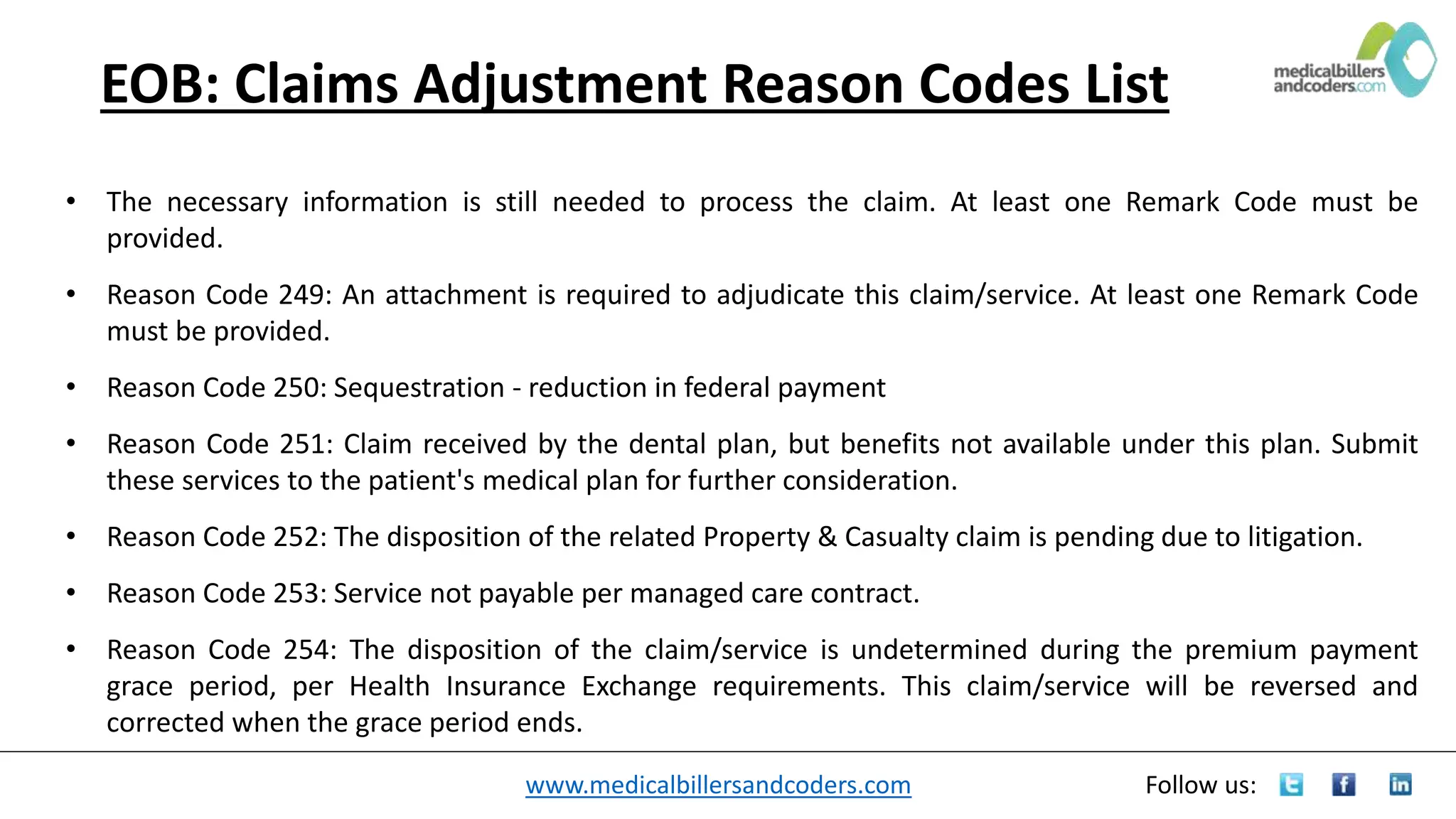
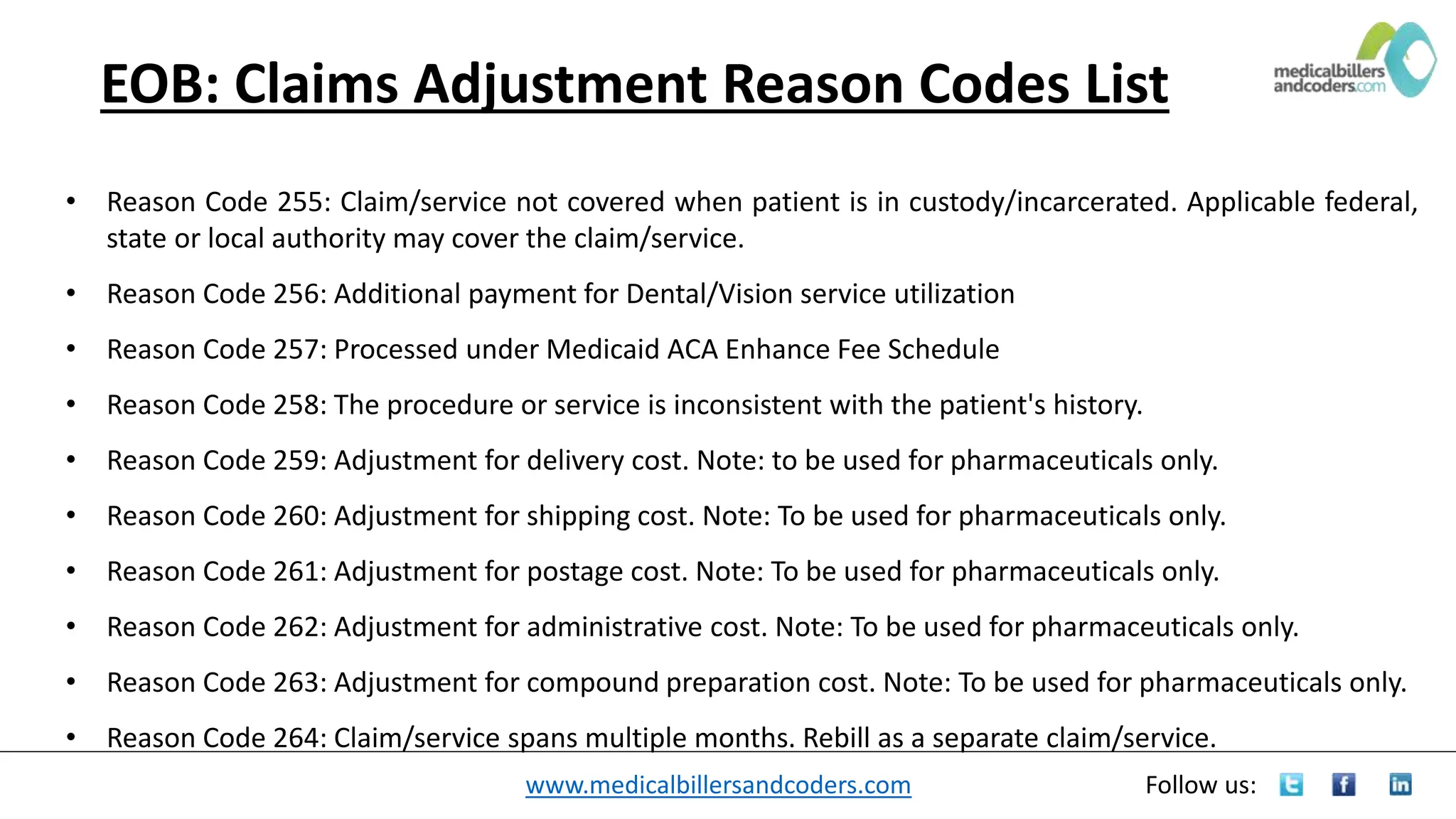
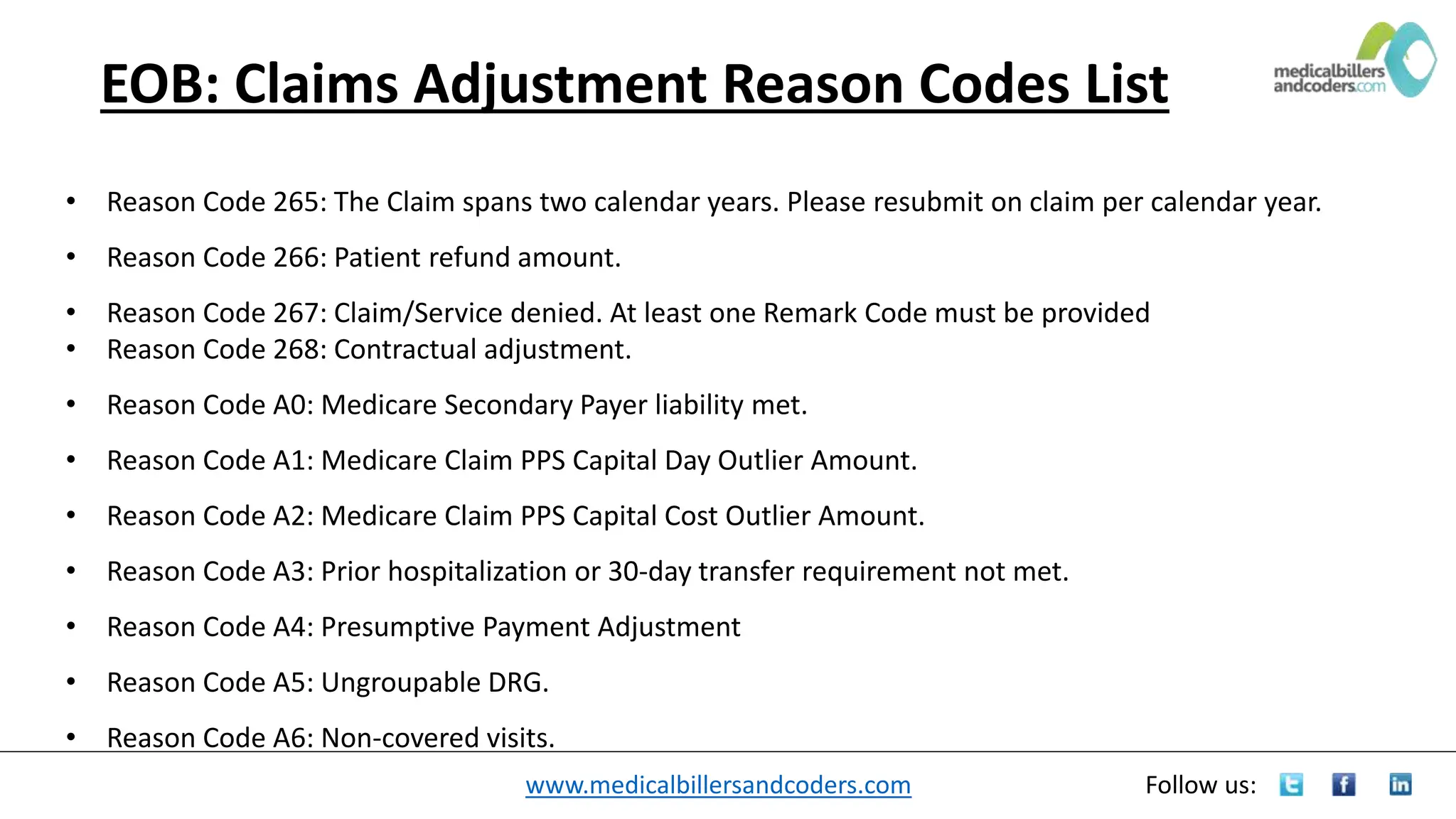
The document outlines a list of claims adjustment reason codes found on an explanation of benefits (EOB), explaining their significance in why claims are adjusted or denied. Each code represents specific reasons related to procedural inconsistencies, coverage issues, and billing errors, providing clear guidance for medical billers and coders. It serves as a comprehensive reference for professionals in the medical billing field to understand and resolve claim adjustments effectively.