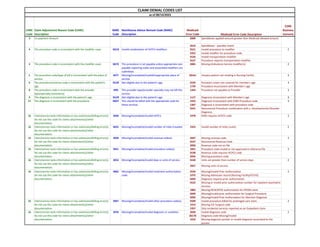
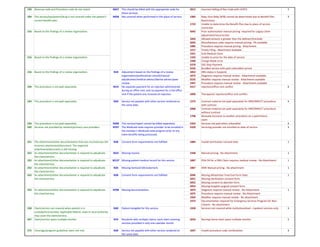
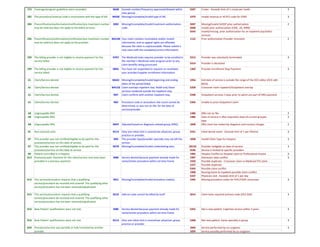
This document contains a list of claim denial codes and descriptions used by Medicaid. It includes codes for issues like missing or invalid information, ineligible procedures, inconsistencies between codes, and coordination of benefits errors. The codes are divided into categories like procedure codes, diagnoses codes, provider identifiers, dates of service, and more. The document provides the code, a description of the issue, and in some cases an explanation code with further details.