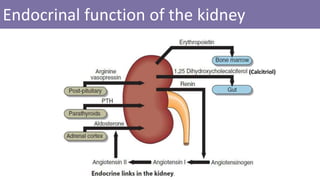
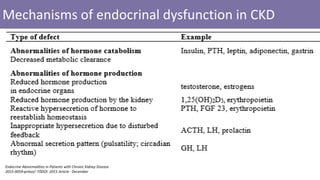
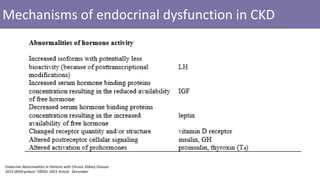
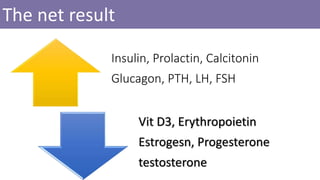
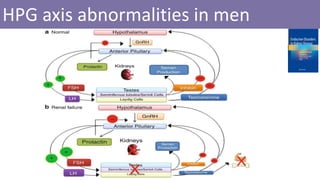
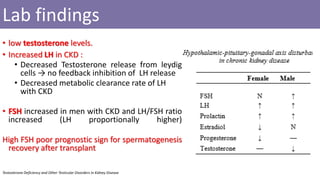
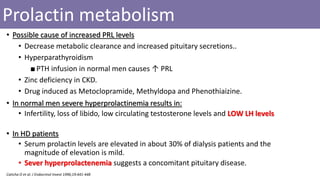
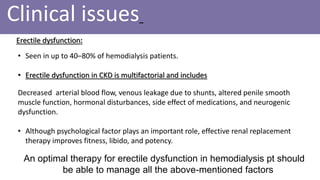
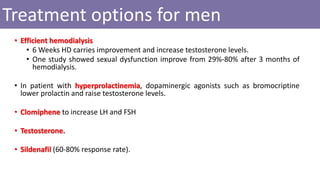
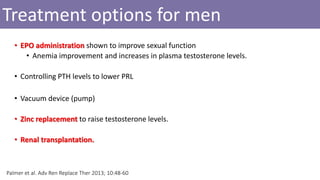
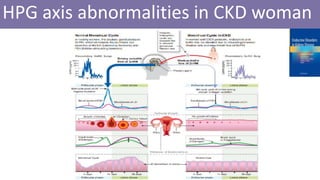
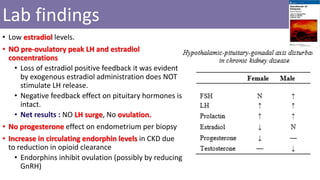
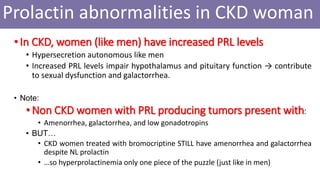
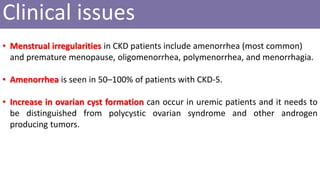
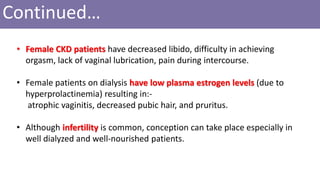
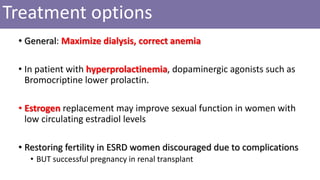
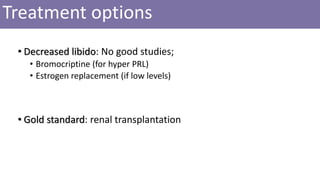
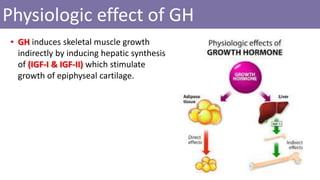
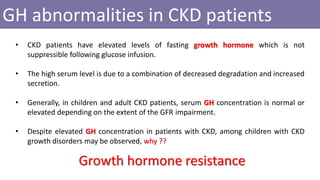
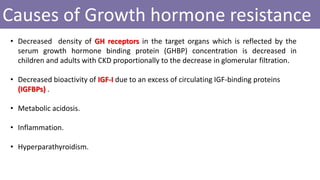
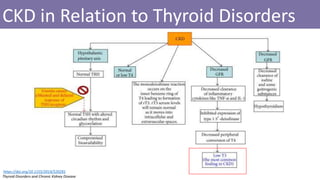
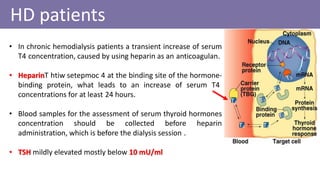
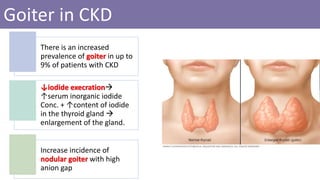
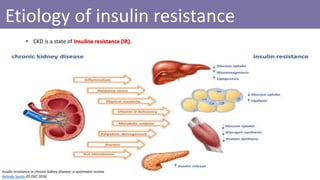
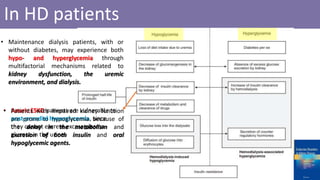
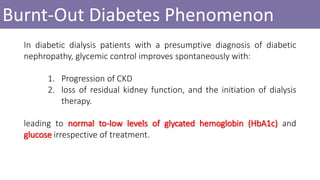
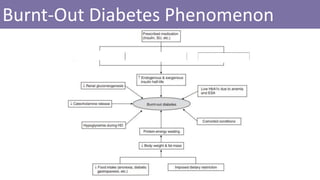
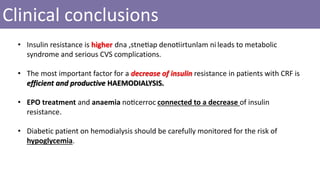
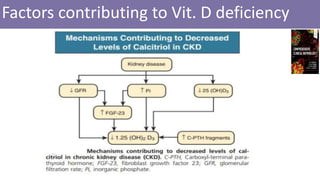
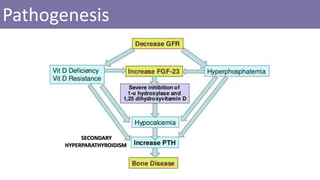
The document summarizes various endocrinal abnormalities seen in patients with chronic kidney disease (CKD) and those undergoing hemodialysis (HD). It discusses dysfunctions of the hypothalamic-pituitary-gonadal axis and thyroid gland in CKD, leading to low testosterone/estrogen, menstrual irregularities, and occasionally goiter. Growth hormone levels are often elevated in CKD due to decreased clearance, but growth is still impaired due to growth hormone resistance. Insulin resistance is also common in CKD. The document outlines treatment options and clinical issues for many of these endocrinopathies.