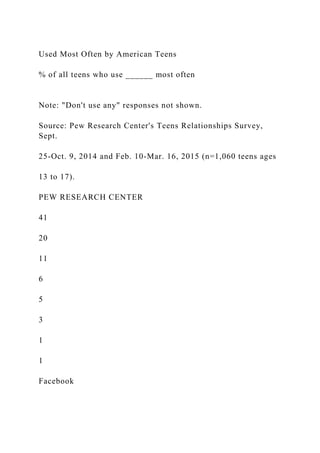
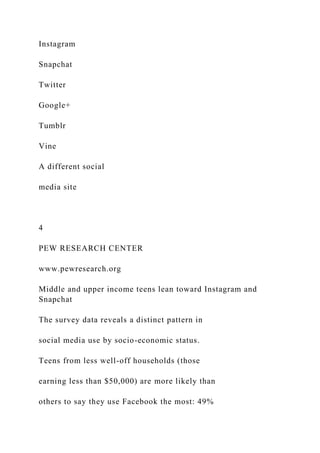
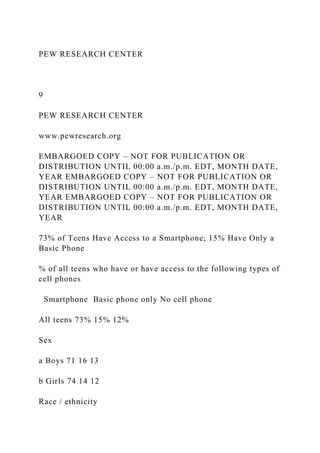
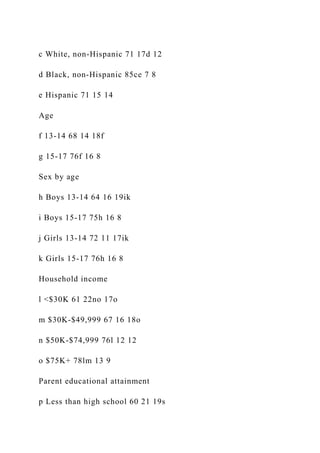
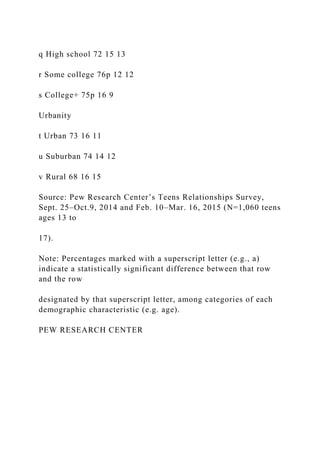
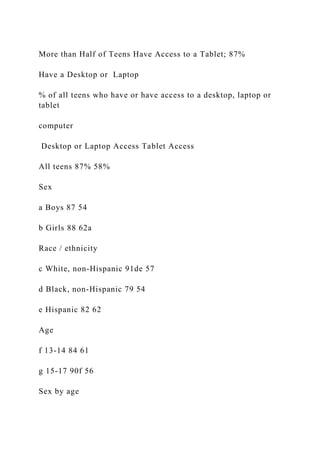
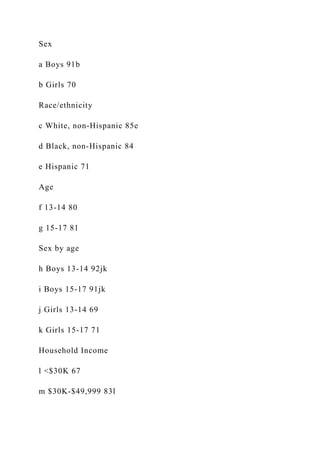
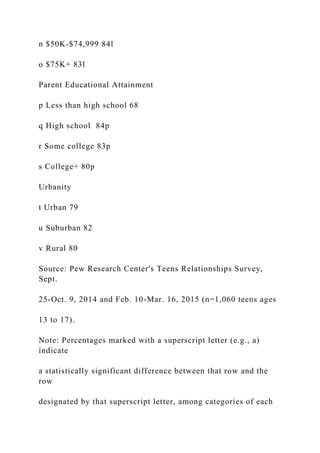
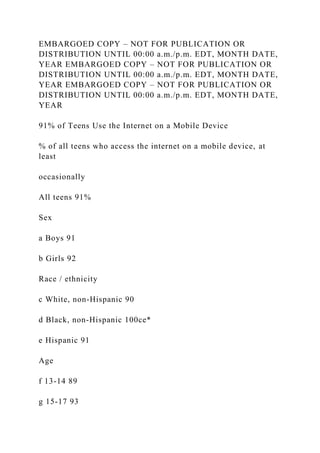
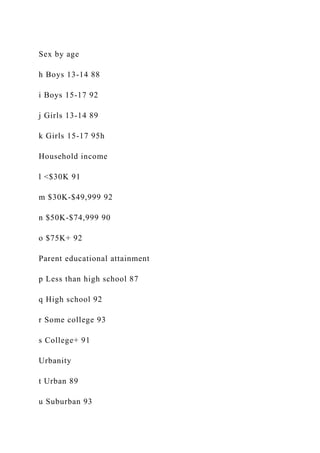
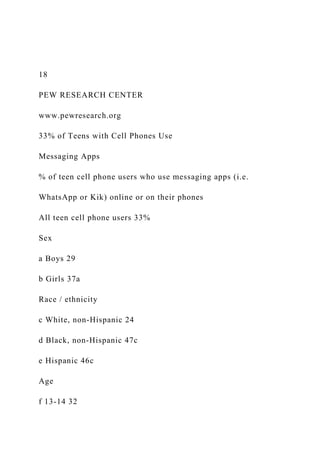
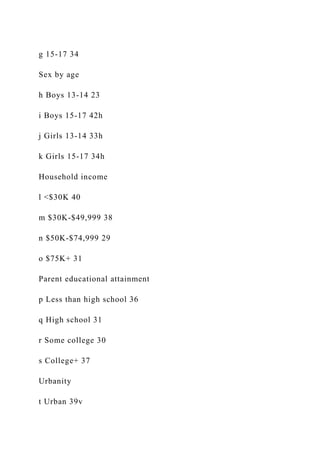
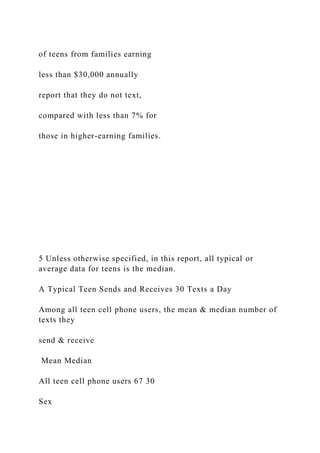
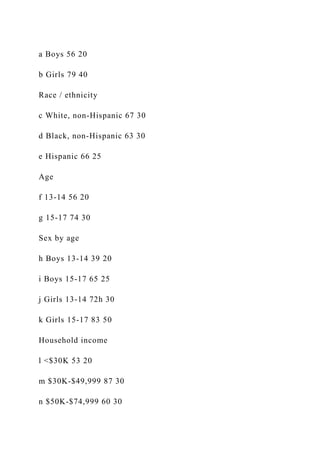
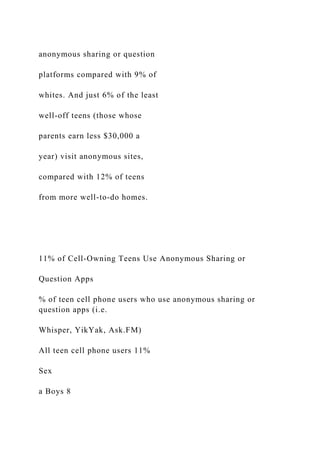
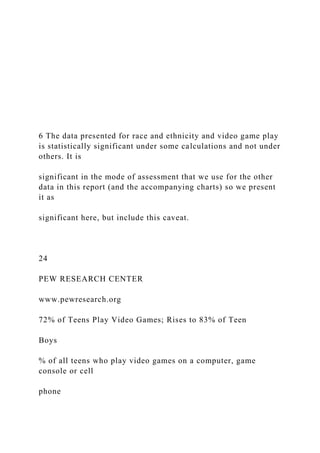
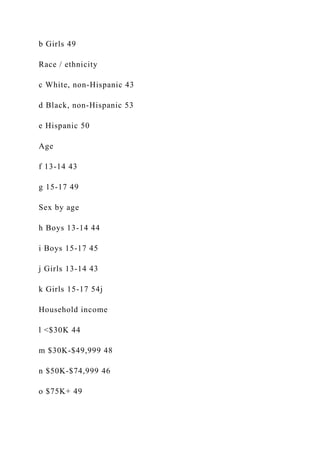
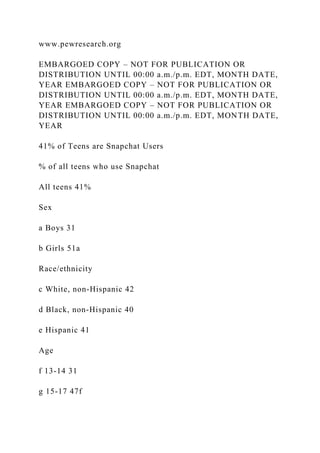
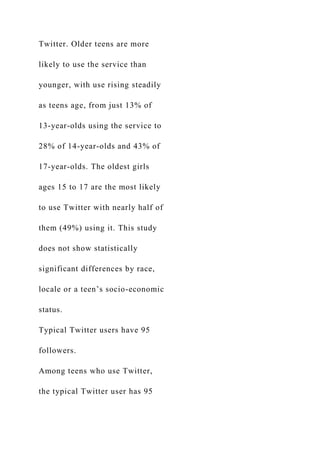
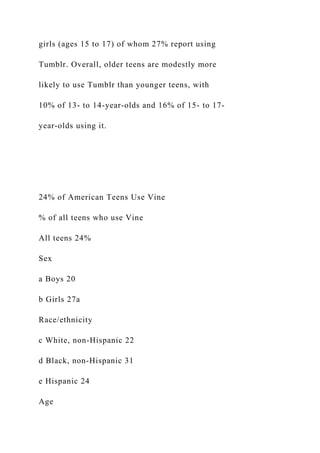
The Pew Research Center's 2015 report highlights that 92% of teens ages 13 to 17 go online daily, with 24% stating they are online 'almost constantly,' primarily driven by smartphone accessibility. Facebook remains the most used social media platform among teens, although Instagram and Snapchat are also popular, particularly among older and wealthier teens. Gender and socioeconomic status significantly influence social media usage patterns, with girls favoring visually-oriented platforms and boys more engaged in gaming, while lower-income teens predominantly use Facebook.




















































![age 13 to 17 years old in the household (1, 2+).
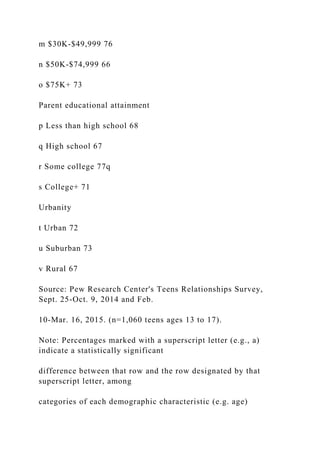
Detailed information on the demographic distributions of the
benchmarks is available upon
request. Please contact Amanda Lenhart at [email protected] for
more information about
the study methodology.
Pew Research Center is a nonprofit, tax-exempt 501(c)3
organization and a subsidiary of The Pew
Charitable Trusts, its primary funder.
mailto:[email protected]
Recommendations for end-of-life care in the intensive care unit:
The Ethics Committee of the Society of Critical Care Medicine
Robert D. Truog, MD; Alexandra F. M. Cist, MD; Sharon E.
Brackett, RN, BSN; Jeffrey P. Burns, MD;
Martha A. Q. Curley, RN, PhD, CCNS, FAAN; Marion Danis,
MD; Michael A. DeVita, MD;
Stanley H. Rosenbaum, MD; David M. Rothenberg, MD;
Charles L. Sprung, MD; Sally A. Webb, MD;
Ginger S. Wlody, RN, EdD, FCCM; William E. Hurford, MD
KEY WORDS: palliative care; intensive care; end-of-life care
T hese recommendations are in-tended to provide
informationand advice for clinicians whodeliver end-of-life care](https://image.slidesharecdn.com/embargoedcopynotforpublicationordistributionuntil0-221026125603-1a0f939e/85/EMBARGOED-COPY-NOT-FOR-PUBLICATION-OR-DISTRIBUTION-UNTIL-0-docx-132-320.jpg)