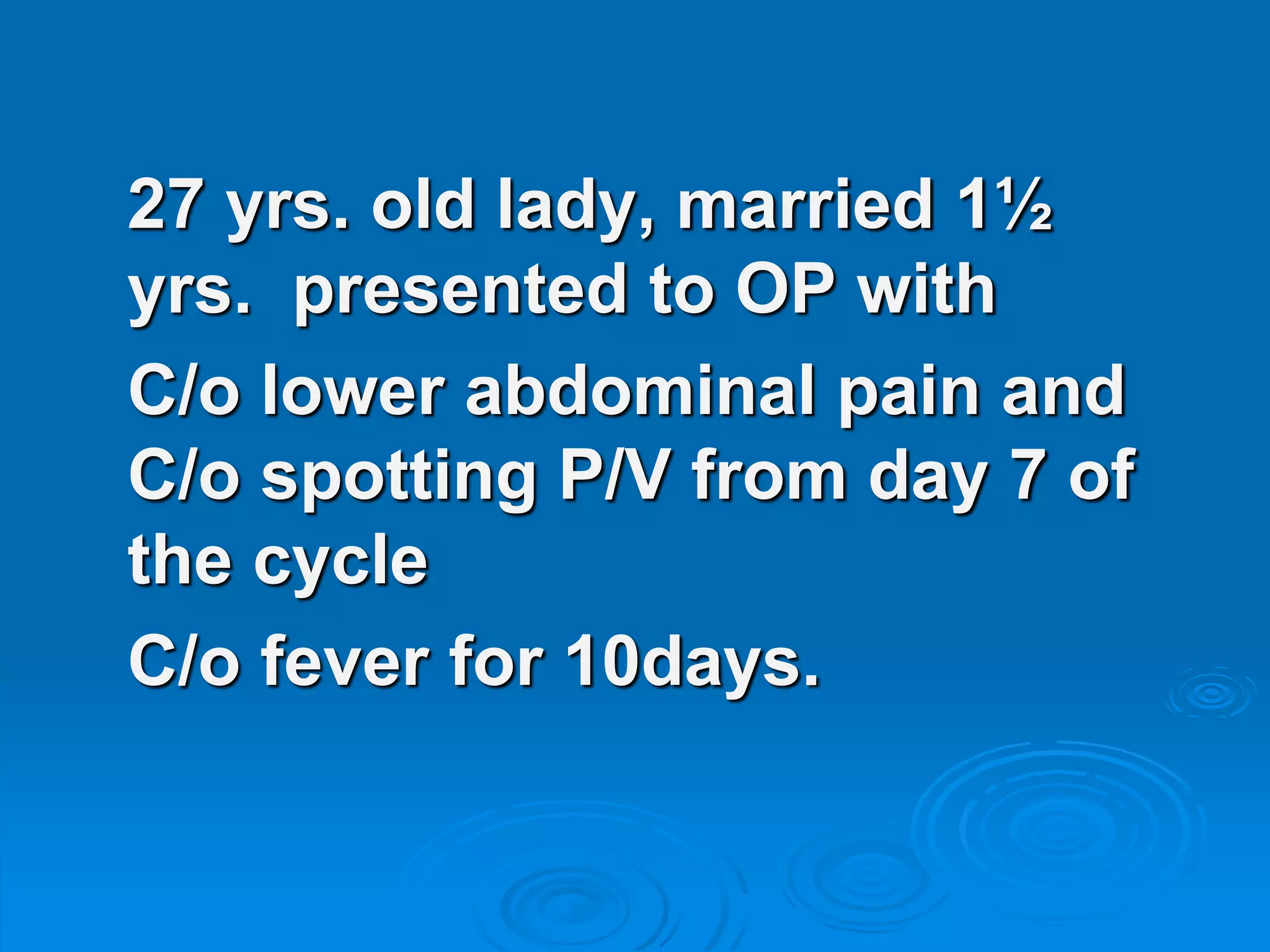
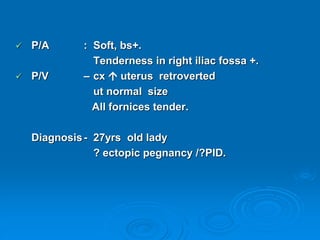
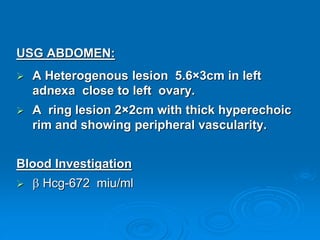
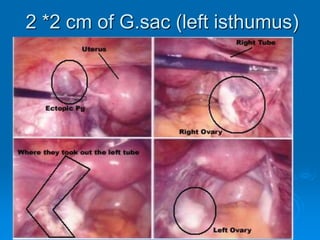
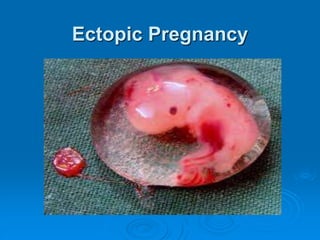
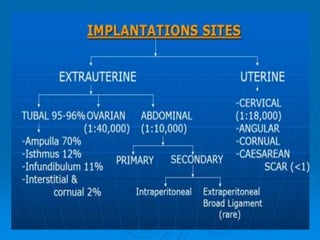
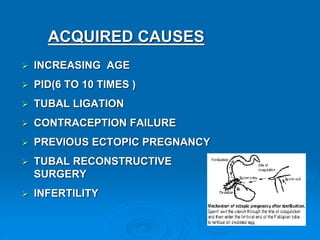
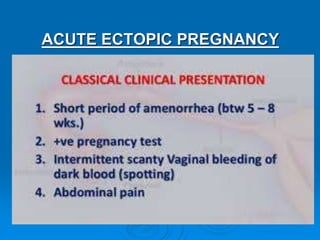
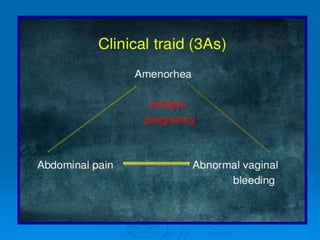
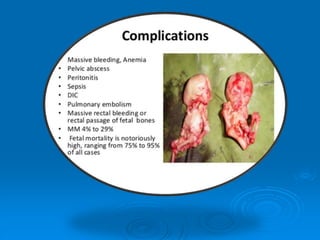
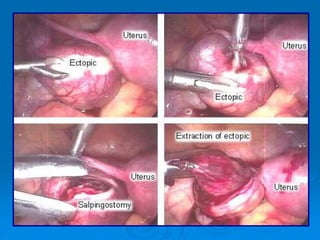
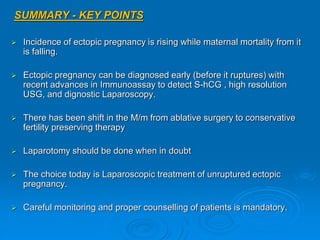
A 27-year-old married lady presented with lower abdominal pain and spotting since day 7 of her menstrual cycle and fever for 10 days. Ultrasound and blood tests confirmed a left tubal ectopic pregnancy. She underwent a laparoscopic left salpingectomy. Ectopic pregnancies occur when the fertilized egg implants outside the uterus, usually in the fallopian tubes, and can be life-threatening if ruptured due to internal bleeding. Advances in early diagnosis with sensitive pregnancy tests, ultrasound, and laparoscopy allow many ectopic pregnancies to be treated conservatively to preserve fertility.