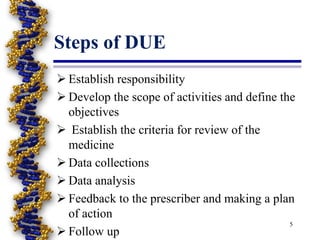
Drug utilization evaluation (DUE) is a systematic, ongoing evaluation of drug therapy that ensures medications are used appropriately and meet current standards of care. The goals of DUE include promoting optimal medication therapy, creating guidelines for appropriate drug use, and controlling costs. The DUE process involves establishing responsibility, developing review criteria, collecting and analyzing data, providing feedback to prescribers, and conducting follow-up evaluations. Drug utilization review (DUR) similarly involves ongoing review of prescribing, dispensing, and drug use, and can be prospective, concurrent, or retrospective to identify problems and improve medication therapy.