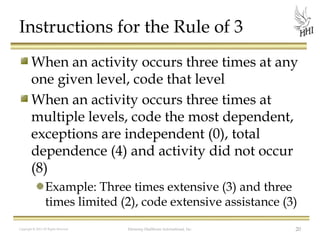
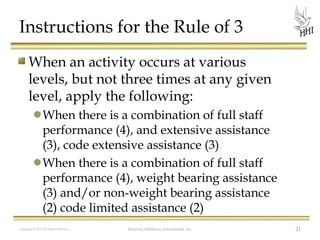
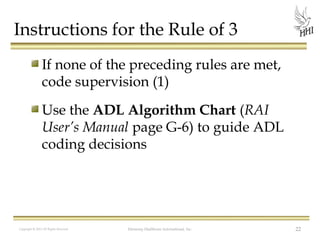
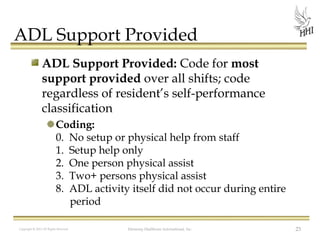
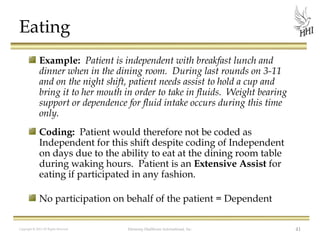
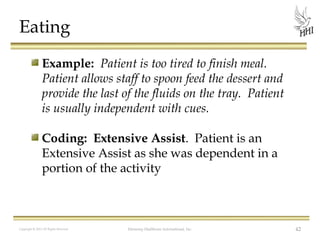
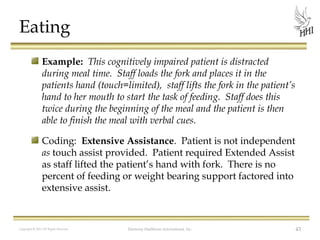
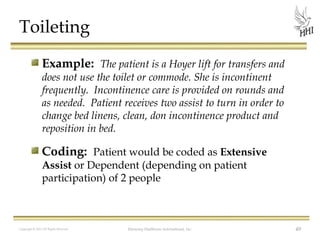
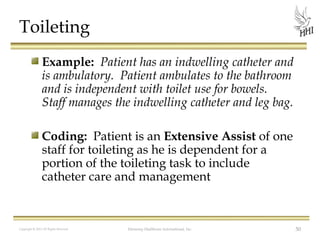
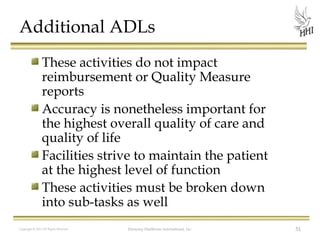
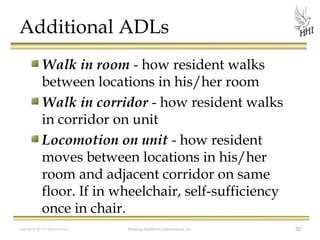
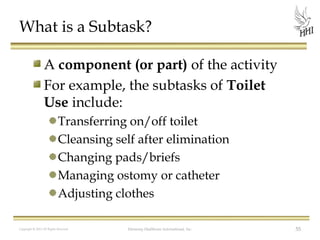
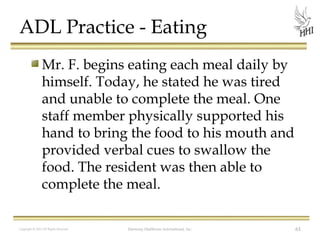
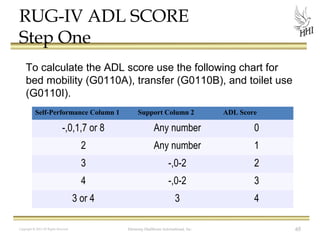
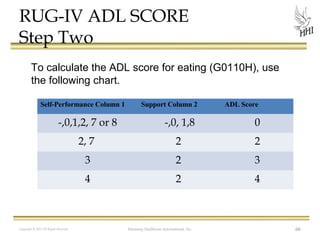
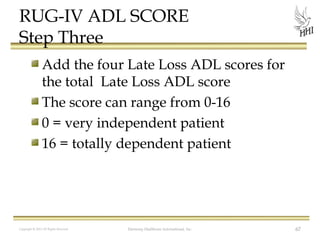
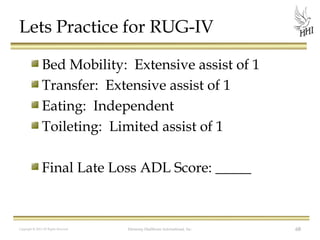
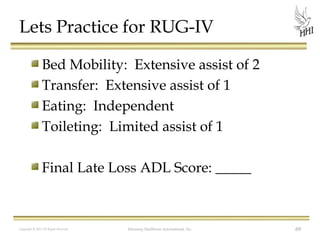
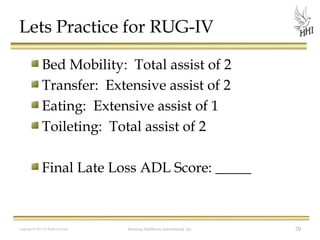
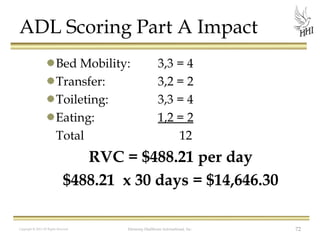
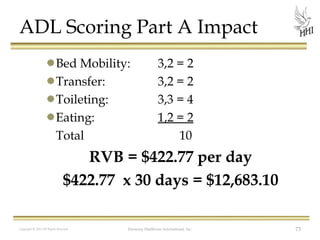
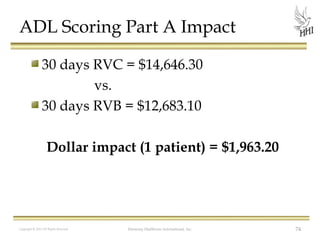
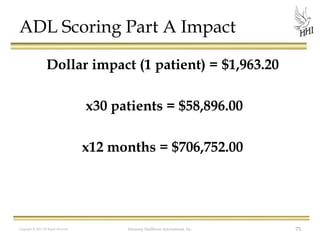
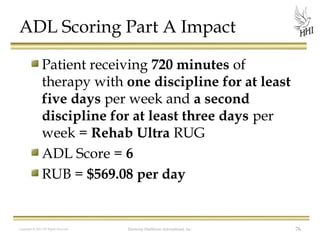
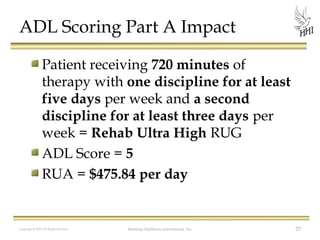
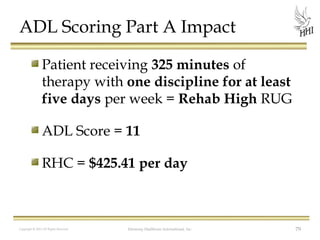
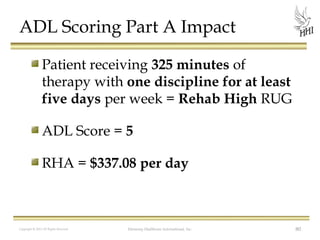
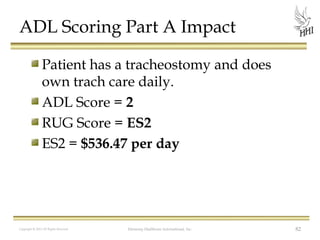
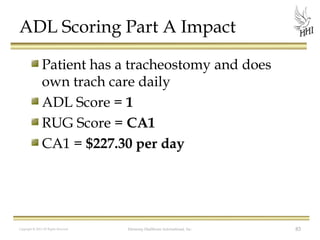
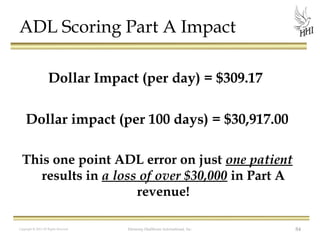
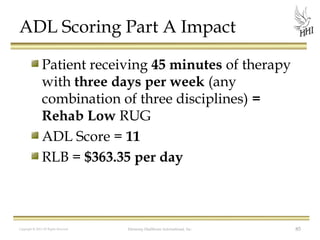
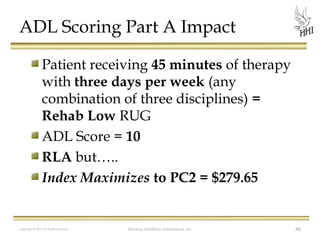
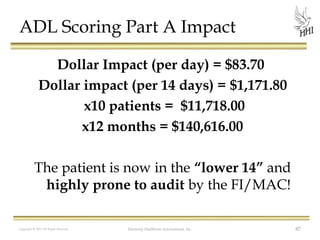
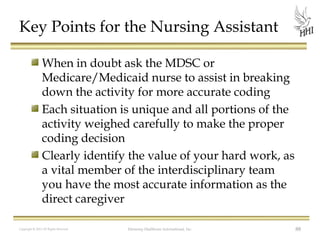
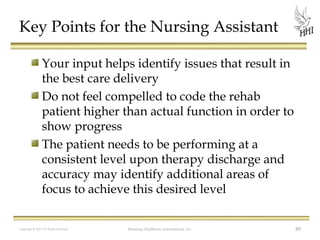
The document outlines the importance of accurate documentation in providing care, specifically focusing on Activities of Daily Living (ADLs) and correct coding for resident support levels. It emphasizes the crucial role of Certified Nursing Assistants (CNAs) in observing and reporting changes in patient function to ensure appropriate care and potential long-term care eligibility. The document provides guidelines for coding ADL performance based on actual support levels received and stresses that documentation should reflect the resident's current capabilities rather than assumptions of their expected abilities.