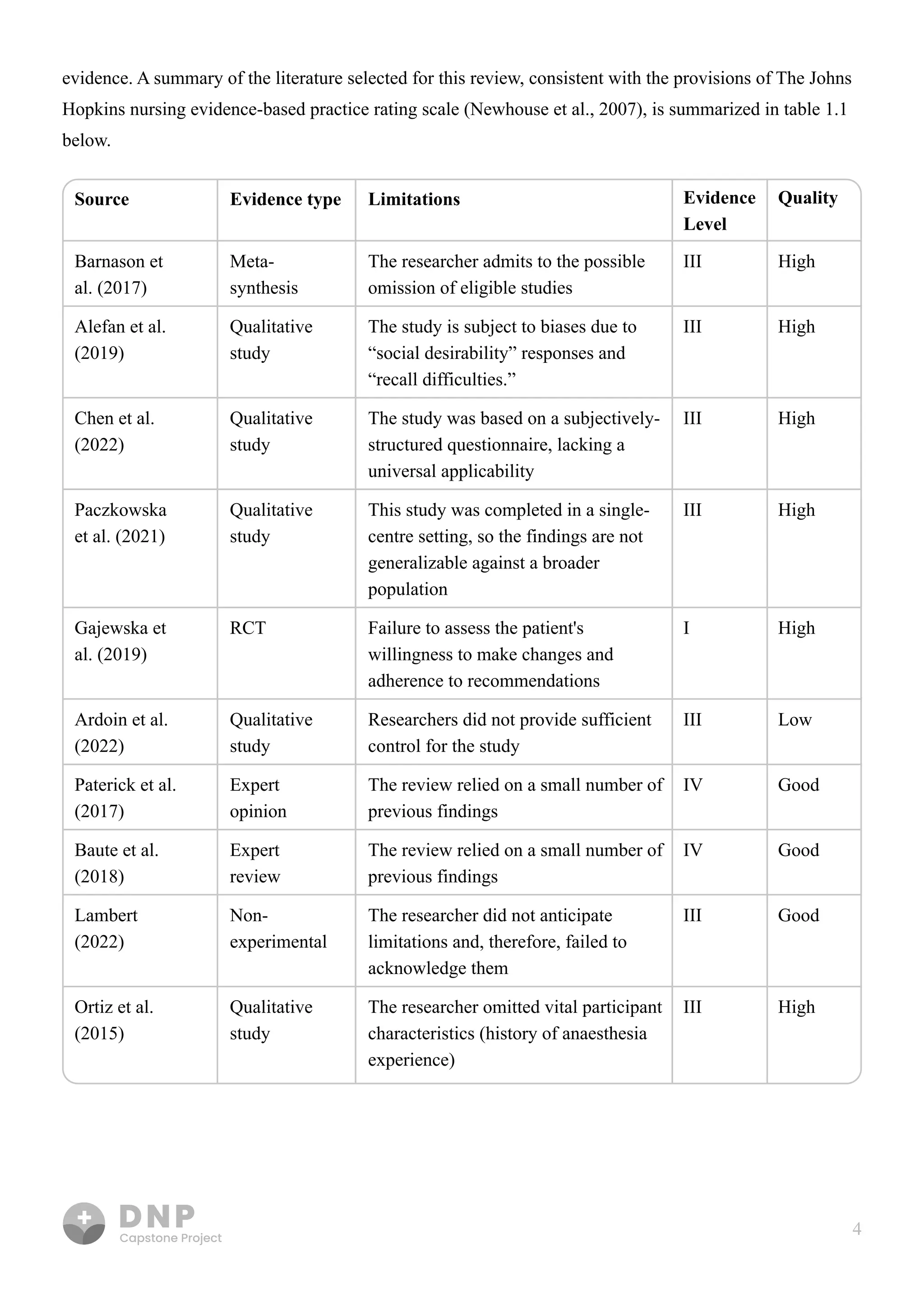
This document discusses the importance of nutritional education, particularly through the DASH diet, in managing hypertension and improving patient outcomes by enhancing nutritional literacy. It reviews existing literature on health literacy and patient education methods, revealing gaps in effective integration of written materials to support patient engagement with dietary guidelines. The synthesis indicates that personalized nutrition education programs significantly influence lifestyle management in hypertensive patients, advocating for targeted educational strategies to improve adherence and blood pressure control.