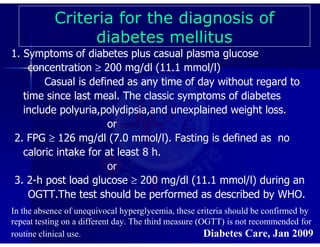
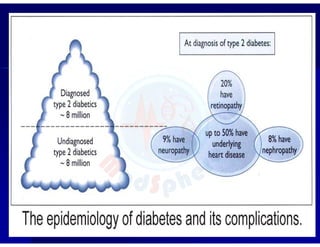
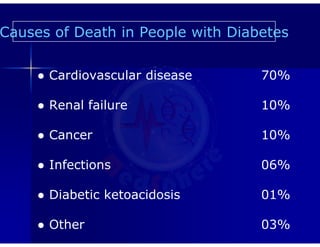
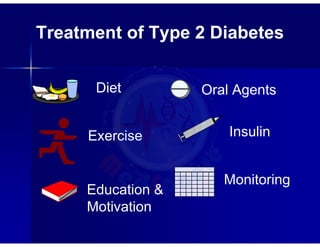
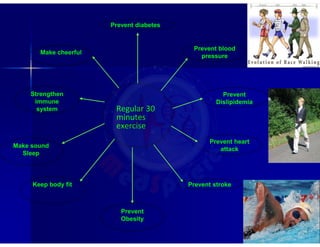
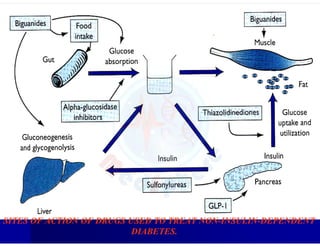
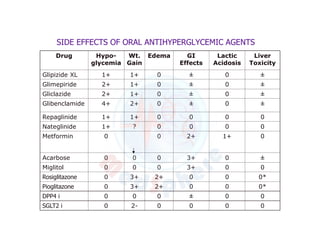
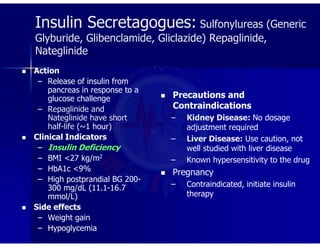
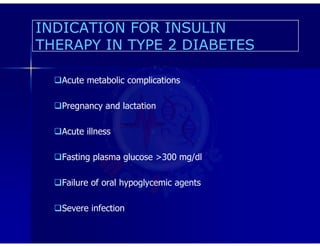
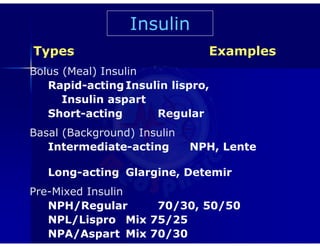
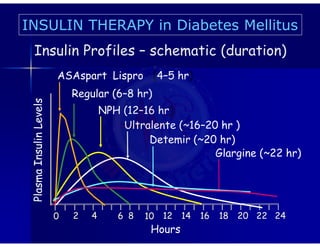
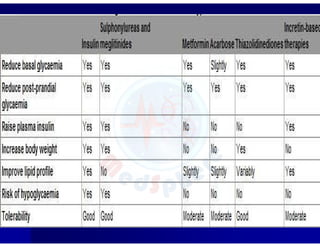
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion or action. Chronic hyperglycemia can cause long term damage to organs like the eyes, kidneys, nerves, heart, and blood vessels. The disease is defined by symptoms of high blood glucose plus a plasma glucose level over 200 mg/dL, a fasting plasma glucose over 126 mg/dL, or a two hour post-glucose load over 200 mg/dL during an oral glucose tolerance test. The main causes of death for people with diabetes are cardiovascular disease and renal failure. Treatment involves lifestyle changes like diet, exercise and education combined with oral medications or insulin to lower blood glucose levels.