This document provides an overview of disturbances in perception, including illusions and hallucinations. It defines illusions as misperceptions of real sensory stimuli, while hallucinations occur in the absence of stimuli. Various types of illusions and hallucinations are described based on etiology, sensory modality, and other factors. Both illusions and hallucinations can affect individuals without psychiatric disorders under unusual conditions like fatigue, sensory deprivation, or grief. The document also discusses other perceptual distortions and how perception is influenced by mood, anxiety, attention, and other psychological factors.
























































































![94
TREATMENT OF MENTAL DISORDERS
HISTORY OF BIOLOGIC TREATMENT OF MENTAL DISEASES
1869 — Chloral hydrate introduced as a treatment for melancholia and mania
1882 — Paraldehyde introduced for a treatment of epilepsy
1903 — Barbiturates introduced as a sedative and anticonvulsant
1917 — Malaria fever therapy of GPI (psychosis of syphilis) [Ju.Wagner von Jauregg]
1927 — Insulin shock for treatment of schizophrenia [M.Sakel]
1934 — Cardiazol (pentylenetetrazol) induced convulsions [L.Meduna]
1936 — Frontal lobotomies [E.Moniz]
1938 — Electroconvulsive therapy [U.Cerletti, L.Bini]
1940 — Phenytoin introduced as anticonvulsant [T.Putnam]
1948 — Disulphiram introduced for treatment of alcohol dependence [E.Jacobsen, J.Hald]
1949 — Lithium introduced for treatment of bipolar psychosis [J.F.Cade]
1952 — Chlorpromazine introduced [J.Delay, P.Deniker]
1953 — Monoanine oxidase inhibitors treatment of depression [G.E.Crain, N.S.Kline]
1956 — Imipramine (the first tricyclic drug) for treatment of depression [R.Kuhn]
1960 — First tranquilizer — chlordiazepoxide introduced [Roche Laboratories, France]
1963 — Valproic acid introduced as anticonvulsant [France]
1963 — Pyracetam introduced [UCB, Belgium]
1965 — First atypical neuroleptic — clozapine introduced
1971-1988— Several serotonin-specific reuptake inhibitors introduced
1986 — Atypical tranquilizer — buspirone introduced
CLASSIFICATION OF PSYCHOPHARMACOLOGICAL DRUGS
Antipsychotics (neuroleptics) — treat the symptoms of psychosis (excitement,
delusions, hallucinations etc.), usually by blocking dopamine and
serotonin receptors.
Antidepressants — treat depressed mood, usually by increasing the activity of](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-94-320.jpg)














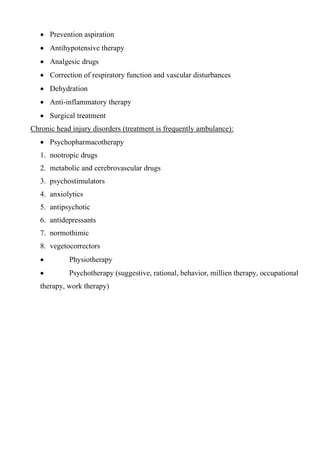
![109
DSM-IV
Diagnostic & Statistical Manual of Mental Disorders
DSM-IV is a multiaxial system that comprises five axes and evaluates the patient along
each. Axis I and Axis II comprise the entire classification of mental disorders: 17 major
groupings, more than 300 specific disorders, and almost 400 categories. In many
instances, the patient has one or more disorders on both Axes I and II. For example, a
patient may have major depressive disorder noted on Axis I and borderline and
narcissistic personality disorders on Axis II. In general, multiple diagnoses on each axis
are encouraged.
Axis I consists of all mental disorders except those listed under Axis II, and other
conditions that may be a focus of clinical attention.
Axis II consists of personality disorders and mental retardation. The habitual use of a
particular defense mechanism can be indicated on Axis II.
Axis III lists any physical disorder or general medical condition that is present in addition
to the mental disorder. The identified physical condition may be causative (e.g., hepatic
failure causing delirium), interactive (e.g., gastritis secondary to alcohol dependence), an
effect (e.g., dementia and human immunodeficiency virus [HIV]-related pneumonia), or
unrelated to the mental disorder. When a medical condition is causally related to a mental
disorder, a mental disorder due to a general condition is listed on Axis I and the general
medical condition is listed on both Axis I and III.
Axis IV is used to code psychosocial and environmental problems that contribute
significantly to the development or the exacerbation of the current disorder (Table 9.1-4).
The evaluation of stressors is based on the clinician's assessment of the stress that an
average person with similar sociocultural values and circumstances would experience
from psychosocial stressors.
Axis IV: Psychosocial and Environmental Problems
✓ Problems with primary support group
✓ Problems related to the social environment
✓ Educational problems
✓ Occupational problems](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-109-320.jpg)




![115
Schisophrenia
(www.feldsher.ru)
(dementia praecox)
Nosological definition
(by Emil Kraepelin and Eugen Bleuler)
1. Aetiology: Endogenous
2. Structure deterioration: no, functional disorder
3. Course: chronic progressive. Outcome: stable
defect of personality
[with autism, formal disorders of thought and
impoverishment of will and emotions, up to apathy,
abulia and schizophrenic dementia (if malignant
cases)].
4. Symptoms and syndromes:
Productive symptoms Negative symptoms
Disorders of sensation
and perception
cenesthopathy,
pseudohallucinations,
depersonalisation,
derealisation
subjective feeling of self-
changing (depersonalisation)
Thought disorders alienation of thoughts,
mentism, thought blocking,
persecutory
delusions (delusion of
control), overvalued ideas,
obsessions
autism, ambivalence,
reasoning, schizophasia,
obscurity of expression,
paralogia, symbolism,
philosophical intoxication,
pontifical woolliness (up to
incoherence) etc.
Affective disorders anxiety, perplexity (acute
delusion), mania or
depression may be, but not
specific
ambivalence, decreased
affect (monotonous,
flattering and incongruity of
affect), apathy](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-115-320.jpg)

![117
f) Thought broadcasting
g) Delusional perceptions
h) All other experiences involving volition, made affects,
and made impulses
ICD-10
According to ICD-10 the diagnosis of schizophrenia cannot be established without 1-
month duration criterion. Conditions clinically equal to schizophrenia but of duration less
than 1 month (whether treated or not) should be diagnosed in the first instance as acute
schizophrenia-like psychotic disorder [F23.2] and reclassified as schizophrenia if
symptoms persist for longer periods.
It is specially marked that 1-moth duration criterion applies only to the specific
symptoms (like listed above) and not to any prodromal nonpsychotic phase.
Also mentioned that diagnosis of schizophrenia should not be made in the presence of
extensive depressive or manic symptoms unless it is clear that schizophrenic symptoms
antedated the affective disturbance.](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-117-320.jpg)


![120
oneiroid states, pseudohallutinations etc.)
Pseudoneurotic schizophrenia
(e.g. cenesthopathic schizophrenia)
F21 — mild disorder which has no connection
with stress and appears with subpsychotic
symptoms (obsession, phobia, depersonalization,
overvalued ideas) and sluggish progression of
schizophrenic negative symptoms.
F20.8 — endogenous form of hypochondria
with strange inner sensations (cenesthopathia).
Types of course
F20.*0 Continuous progression
F20.*1 Progression with acute attacks [German - Schub]
F20.*3 Periodic (recurrent)
F21 Special type with slow (sluggish) progression — In ICD-10 Schizotypal disorder
(eccentric, bizarre behavior — German – Verschroben).
progression with acute attacks
slow (sluggish) progression
periodic (recurrent)
with slow progression
P +
N -
—
P +
N -
—
P +
N -
—
continuous progression
P +
N -
—](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-120-320.jpg)
![121
ORGANIC MENTAL DISORDERS F00 - F09
SPECIFIC SYMPTOMS (Walter-Buel H. triad):
1. Difficulties in retention (up to amnesia – F04)
2. Difficulties in understanding (up to dementia – F00-F03)
3. Difficulties in keeping feelings in (e.g. disphoria or emotional incontinence)
ADDITIONAL SYMPTOMS:
4. Changes in personality and general behaviour [F07]
5. Neurological signs and symptoms
6. Asthenia (emotional hyperaesthetic syndrome)
7. Somatic symptoms (headache etc.)
8. Weather sensitivity.
METHODS OF DIAGNOSTIC:
✓ EEG](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-121-320.jpg)
![5
Hallucinations in delirium
(www.feldsher.ru)
✓ CT (Computer Tomography) or
MRI (Magnetic Resonance Imaging)
✓ Ophthalmologist examination
✓ Neurologist examination
✓ Rheoencepalography
✓ Doppler ultrasound
✓ Cerebro-spinal fluid (CSF) tests
✓ Neuropsychological tests
PSYCHO-ORGANIC SYNDROME
A heterogeneous group of states usually
observed in individual stages of the course
of various organic diseases. In the first
stages of development, increasing manifestations of mental weakness and increased
fatigability are usually discovered. Later these are joined by disorders of attention,
memory and intellectual activity, psychopathic like disturbances, and various emotional
disorders. Delirium [F05], true hallucinations and delusional disturbances [F06] may be
observed. Delusional disturbances are fleeting and fragmentary, with no tendency
towards systematization, and they vary in content. Affective disorders fluctuate from an
uplifted mood with euphoria to depression and increased irritability, peevishness,
sometimes with an overlay of dysphoria and maliciousness.
DEGENERATIVE
CEREBRAL
DISEASES
Alzheimer’s disease [F00, G30] – degenerative disease with
insidious onset at age 55—65 or later (occur in women 3-5
times more often than in men) with prominence of features of
parietal and temporal lobe damage (loss of memory, apraxia,
acalculia, dysgraphia, dysartria). It develops slowly but
steadily. Formal complaints coexist with poor insight (total](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-122-320.jpg)
![Рисунок 2 – Деперсонализация при нервной анорексии
dementia).
Pick’s disease [F02, G31] – a progressive dementia with onset
at age 50-60 with features of selective atrophy of frontal and
temporal lobe (apathy, euphoria, severe character changes,
verbal and motor stereotypy). The course is rather malignant;
no sense of illness exists (total dementia).
CEREBRAL
ARTERIOSCLEROSIS
System disease with slow progression and evident waving
course. Cerebral symptoms coexist with features of ischaemia
of heart or extremities. The first symptoms are asthenia and
hypomnesia. Dementia appears later, insight is rather good
(partial dementia – F01)
TUMOURS Neurological symptoms are common in onset (paralysis,
disorders of co-ordination of movement, disorders of vision,
epileptic seizures etc.). If the frontal lobes are impaired, the
changes of character, apathy and poor insight are typical. The
symptoms of cranial hypertension are common (headache
with retching increasing by the morning, clouding of
consciousness).
TRAUMA Acute or chronic regressive course. Stages are: loss of
consciousness (up to coma), acute period (sometimes with
acute psychosis, for example delirium), convalescence
(through the stage of asthenia), consequences (cerbrasthenia,
Korsakov’s syndrome, dementia, epileptic seizures,
personality disorder).
INFECTIONS GPI (general paralysis of insane – F02.8, A52.1) – syphilitic
psychosis which appears in some patients in 10-15 years after
infection. The symptoms of encephalitis are the loss of
insight, euphoria, dementia, severe personality changes,
delusions of grandeur. Neurological signs: Argyll-Robertson
symptom, asymmetry of tendon reflexes. Wassermann test is](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-123-320.jpg)
![positive in 95% of patients. Treatment: antibiotics,
iodotherapy, bismuth drugs.
AIDS dementia [F02.4, B22.0] – up to total is common in
terminal phase. Treatment is symptomatical.
EPILEPSY G40
Nosological definition:
1. Aetiology: Endogenous
2. Structure deterioration:
organic
3. Course:chronic
progressive.
Outcome: Epileptic dementia (if malignant cases).
4. Symptoms and syndromes:
Productive symptoms: rather different but ever paroximal.
Negative symptoms: stable defect of personality with egocentrism (selfishness),
circumstantiality (stiffness), emotional rigidity and
explosivity.
Epilepsy
(rus-img.com)](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-124-320.jpg)




![Реактивная депрессия F32 – Depressive episode
Посттравматическое стрессовое
расстройство (ПТСР)
F43.1 – Post-traumatic stress disorder
Реактивный параноид
F23.31 – Other acute predominantly
delusional psychotic disorders (including
paranoid reaction)
NEUROSES (неврозы)
Неврастения
F48.0 – Neurasthenia
Невроз навязчивых состояний
F40 – Phobic anxiety disorders,
F41 – Other anxiety disorders
(including panic disorder),
F42 – Obsessive-compulsive disorder,
F45.2 – Hypochondriacal disorder
(including nosophobia)
Истерический невроз
F44 – Dissociative [conversion] disorders,
F45 – Somatoform disorders
Ипохондрический невроз
F45.2 – Hypochondriacal disorder
(nondelusional)
Депрессивный невроз
F34.1 – Dysthymia,
F43.2 – Adjustment disorders,
F43.1 – Post-traumatic stress disorder
Acute Stress Induced Psychoses
Nosological definition:
1. Aetiology: psychogenous, the result of acute irresistible stressors concerning the
primary personal needs (safety, health, honour, freedom and so on)](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-129-320.jpg)

![the kind of neurosis depends upon the type of personality.
‘intellectual’ type with predominance of the second set of conditioned stimuli (language,
logic, operating with symbols) over the first is common for patients with
obsessive-phobic neurosis
‘artistic’ type with predominance of the first set of conditioned stimuli (emotions,
sensations and intuition) over the second is common for patients with hysteric
neurosis
According to S.Freud
the symptoms of neuroses represent unconscious psychological defense against the
irresistible internal conflicts (often sexual problems). Unconscious motives are the cause
of the poor insight and resistance against the treatment.
CLINICAL FORMS
Neurasthenia appears with the symptoms of asthenia (fatigability in combination with
irritability) that are linked to meaningful psychological stressors.
Symptoms:
Psychological: tiredness, poor memory, sleep disorders, lack of restraint,
psychological sensibility (appeared with tears or verbal violence).
Somatic: functional pain (headache, stomachache, and backache), arterial hypo- or
hypertension, palpitation, sweating, linked to psychological troubles or
physical difficulties.
Hysteria (dissociative [conversion] disorders, somatoform disorders, somatization
disorder) is characterized by physical or psychological symptoms for which no physical
cause can be identified but which are linked to meaningful psychological stressors. The
symptoms may help patients unconsciously deal with internal conflicts. It is more
common in women and patients with demonstrative (histrionic) features of personality.
It is strongly recommended to make special investigation to exclude any other cause of
the somatic symptoms because about 30% of patients with preliminary diagnose of
hysteria are later diagnosed with organic disorders (cancer, multiple sclerosis,](https://image.slidesharecdn.com/disturbancesinperception-221018182626-9693a7bd/85/DISTURBANCES-IN-PERCEPTION-pdf-132-320.jpg)