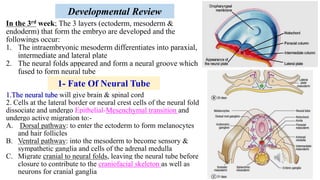
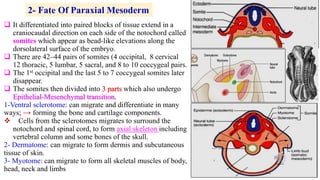
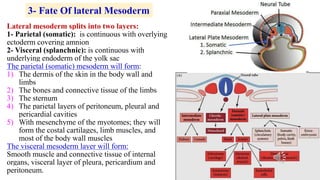
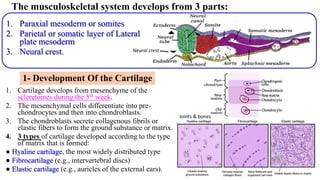
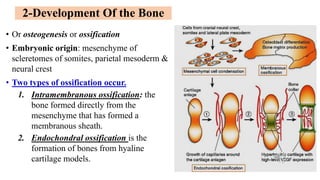
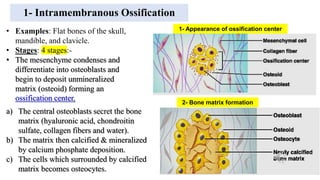
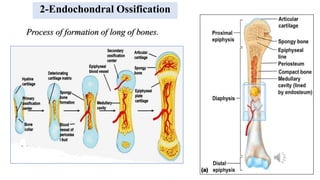
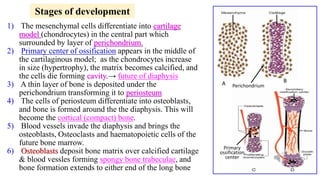
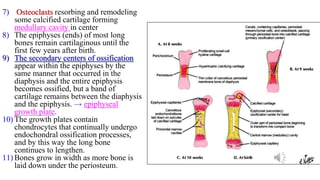
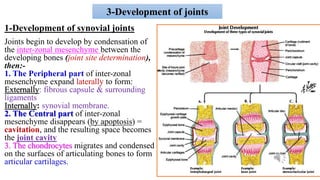
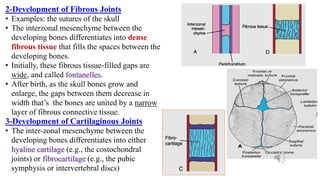
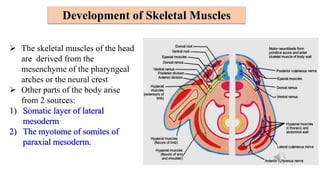
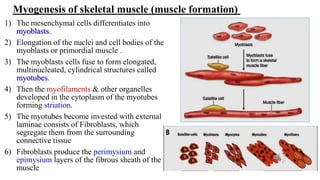
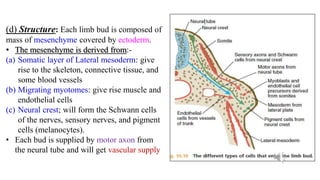
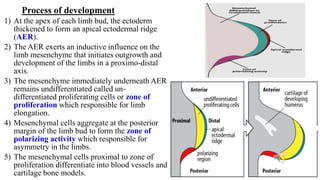
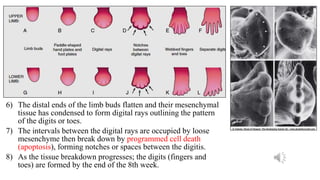
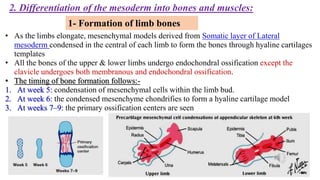
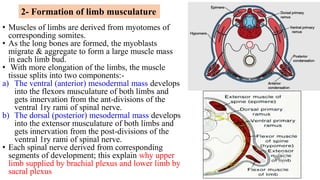
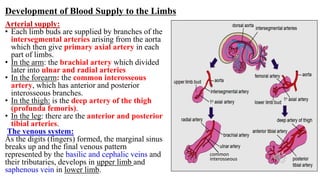
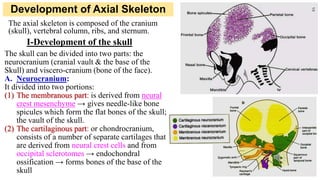
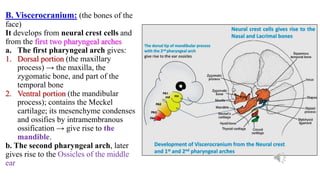
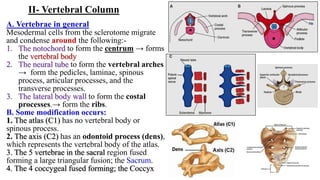
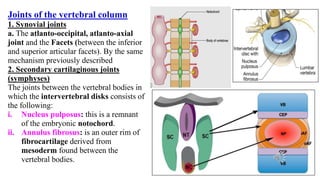
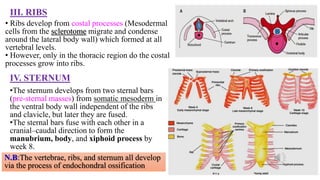
The document outlines the development of the musculoskeletal system, covering the formation of bones, cartilage, joints, and muscles. Key processes include differentiation of mesoderm layers, formation of somites that contribute to skeletal structures, and ossification methods such as intramembranous and endochondral ossification. Additionally, it details the patterning and growth of limb buds, skeletal muscle formation, and the development of nerve supplies to the limbs.