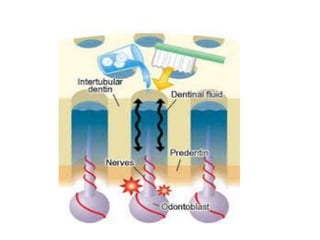
Dentin hypersensitivity is characterized by short, sharp pain from exposed dentin in response to stimuli like heat, cold, sweet foods, or toothbrushing. It occurs when gums recede or enamel is lost, exposing open dentin tubules. The hydrodynamic theory explains that stimuli cause fluid movement in dentin tubules, activating nerve endings and causing pain. Treatment focuses on desensitizing nerves with potassium nitrate toothpaste or occluding tubules with agents like fluoride, CPP-ACP, or resins to block fluid flow and pain signals.