Death and dying practice
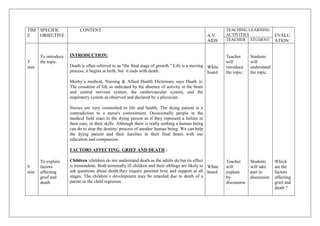
- 1. TIM SPECIFIC CONTENT TEACHING LEARNING E OBJECTIVE A.V. ACTIVITIES EVALU AIDS TEACHER STUDENT ATION To introduce INTRODUCTION: Teacher Students 3 the topic. will will min Death is often referred to as ―the final stage of growth.‖ Life is a moving White introduce understand process, it begins at birth, but it ends with death. board the topic. the topic. Mosby’s medical, Nursing & Allied Health Dictionary says Death is: The cessation of life as indicated by the absence of activity in the brain and central nervous system, the cardiovascular system, and the respiratory system as observed and declared by a physician. Nurses are very committed to life and health. The dying patient is a contradiction to a nurse's commitment. Occasionally people in the medical field react to the dying person as if they represent a failure in their care, or their skills. Although there is really nothing a human being can do to stop the destiny/ process of another human being. We can help the dying patient and their families in their final hours with our education and compassion. FACTORS AFFECTING GRIEF AND DEATH : To explain Children :children do not understand death as the adults do but its effect Teacher Students Which 9 factors is tremendous. Both terminally ill children and their siblings are likely to White will will take are the min affecting ask questions about death.they require parental love and support at all board explain part in factors grief and stages. The children’s development may be retarded due to death of a by discussion affecting death. parent or the child regresses. discussion . grief and .. death ?
- 2. young and middle aged people : They approach death reluctantly. Separation from loved ones is difficult to accept .The elderly person, however, often looks upon death with less dread. For him death may represent peace and relief from suffering. For the person who has always been healthy and suddenly becomes critically ill,death is often feared. Family : The patient’s families react to death and dying in a variety of a ways. They feel lost as to what to say, and how to act in an aggressive manner towards the nurse and the health agency when the patient is critically ill or after death. This can be an expression of feelings of helplessness and frustration. Patient : Patients react to death in many ways.some people frankly express their feelings and their fears while fears while others hide them in an air if superficially.some become aggressive , hostile or withdrawn;others maintain a composure , which hides many anxieties. Nurse : The nurse also reacts in different ways to the dying patient and to death. Her reactions largely depends on her own past experiences , beliefs and needs. She has to be very alert with relatives covert or overt actions of cultural practices during the last stages. Socio – economic factors :
- 3. A bereaved family may suffer more acutely if there is no other earning member in the family. They not only have loss of a loved one , but also economic loss that may further disrupt family life. Cultural influences : Culture also influences an individual’s expression of grief. In many families , grief is a private matter shared only with the family. Many individuals internalise their feelings of grief and may not express grief or feelings of loss to others.on the other hand , cultural background may necessitate the family to display emotion and distress with loud weeping and mourning which may disturb the other patients in the ward. MEETING THE NEEDS OF GRIEVING AND DYING INDIVIDUALS : Teacher To discuss White will how will 10 the needs of The client’s needs are met by attending the following aspects like : board discuss Students you min dying needs of will provide individuals. Physical needs : dying participate care to individual in dying s by discussion person ? asking Dying may take a few minutes, days or weeks. There is a general questions . slowing down of the bodies' processes as a person is dying. They become weak; levels of consciousness may change. It is very important to allow the patient as much independence as possible. As they become weaker or less responsive the nursing team will need to help with basic needs. As the death nears the patient might become totally dependent on the nursing staff for all of their ADL’s. Every effort is given to provide the best care, physically and psychological to a dying patient. This person needs be allowed to die in
- 4. comfort and with DIGNITY… VISION, HEARING and SPEECH- Vision may become blurred and gradually fail, this person will automatically turn towards the light, a very dark room may frighten them. Keeping some light in the room is important, but not real bright lights. The eyes may stay half-open, this will cause dryness and accumulation of secretions in the corners, and frequent eye care is necessary. Always talk to the patient and let them know you are there and keep some light in the room. Hearing is the last sense to go, ALWAYS remember the patient can hear you even when you think there is no way they could, they can! So talk to them, continue to explain what you are doing and why, keep your normal tone of voice, offer words of reassurance and comfort. Remember to never offer false promises. MOUTH, NOSE and SKIN- oral hygiene is a must! A dying person’s mouth many times become very dry and their lips crack. Mouth care is important and needs to be done frequently with glycerin swabs, or toothettes. You do not want to put a lot of water, or fluids in the dying person's mouth. Many times they are unable to swallow and too much fluid can cause them to aspirate. When giving mouth care always have the head of the bed up and their heads turned to the side. Part of mouth care is applying lubricant to the patients' lips. The nostrils may become dry or crusted from drainage or oxygen, assess these areas frequently. CIRCULATION decreases and then fails. Body temperature may increase as death approaches. Even though the body temperature goes up the skin becomes cool, pale, and mottled. Perspiration increases, many times profusely. Good skin care, bathing, and prevention of decubitis ulcers are very important nursing measures. Positioning the patient frequently and keeping them comfortable as
- 5. possible, you may use pillows to help with positioning and to avoid skin to skin contact. ELIMINATION- the dying person may become incontinent of bowel and bladder. Remember DIGNITY. Bed protectors or attends may be needed. Perineal care is very important. Psychological needs : Patients' insight into their condition should be assessed. Issues relating to dying and death should be explored appropriately and sensitively. Clients differ in their emotional responses when recognizing that death is inevitable. some person speak of their fears of death. Responses include fear of the unknown , separation , pain of leaving loved ones ,loss of dignity and so on. .nurse should be involved in giving hope ,while helping the client to deal with reality. No matter what the behaviour of client is,it should be accepted by the nursing staff. A fear of isolation of having to face the death alone is a primary fear of the dying person . yhe nurse supports the client by providing her/him full attention.presence of members of the family needs to be encouraged. Social needs : The family's insight into the patient's condition should be assessed and issues relating to dying and death explored appropriately and sensitively. The family should be told that the clinical expectation is that the patient is dying and will die. Use of ambiguous language such as ―may not get better‖ can lead to misinterpretation and confusion. A constant source of
- 6. frustration and anger voiced by bereaved relatives is that no one sat down and discussed the fact that their loved one was dying. If relatives are told clearly that the patient is dying they have the opportunity to ask questions, stay with the patient, say their goodbyes, contact relevant people, and prepare themselves for the death. Relatives of patients dying in the community should be given contact telephone numbers so that they have access to help and advice on a 24 hour basis. Spiritual needs : Sensitivity to the patient's cultural and religious background is essential. Formal religious traditions may have to be observed in the dying phase and may also influence care of the body after death. After the patient's death, relatives should be dealt with in a compassionate manner. A leaflet explaining issues related to grieving can be helpful. Hospice care : Hospice care is end-of-life care provided by health professionals and . volunteers. They give medical, psychological and spiritual support. The goal of the care is to help people who are dying have peace, comfort and dignity. The caregivers try to control pain and other symptoms so a person can remain as alert and comfortable as possible. Hospice programs also provide services to support a patient's family. Usually, a hospice patient is expected to live 6 months or less. Hospice care can take place At home
- 7. At a hospice center In a hospital In a skilled nursing facility STAGES OF DYING : To describe Teacher Students Which 7 stages of Clients’ reaction to impemding death is unique to everyone,Dr .elizabeth will will are the min dying. kubler-ross studied responses to death and her findings have been used lcd explain verbalise stages of using a.v stages of dying ? extensively by nursing and other professionals. According to kubler aids. dying. ross, the stages of dying are (1) Denial and isolation (2) Anger (3) Bargaining (4) Depression (5) Acceptance 1. Denial and Isolation The first reaction to learning of terminal illness or death of a cherished loved one is to deny the reality of the situation. It is a normal reaction to rationalize overwhelming emotions. It is a defense mechanism that buffers the immediate shock. We block out the words and hide from the facts. This is a temporary response that carries us through the first wave of pain. 2. Anger As the masking effects of denial and isolation begin to wear, reality and its pain re-emerge. We are not ready. The intense emotion is deflected from our vulnerable core, redirected and expressed instead as anger. The anger may be aimed at inanimate objects, complete strangers, friends or family. Anger may be directed at our dying or deceased loved one.
- 8. Rationally, we know the person is not to be blamed. Emotionally, however, we may resent the person for causing us pain or for leaving us. We feel guilty for being angry, and this makes us more angry.. The doctor who diagnosed the illness and was unable to cure the disease might become a convenient target. Health professionals deal with death and dying every day. That does not make them immune to the suffering of their patients or to those who grieve for them. Do not hesitate to ask your doctor to give you extra time or to explain just once more the details of your loved one’s illness. Arrange a special appointment or ask that he telephone you at the end of his day. Ask for clear answers to your questions regarding medical diagnosis and treatment. Understand the options available to you. Take your time. 3. Bargaining The normal reaction to feelings of helplessness and vulnerability is often a need to regain control– If only we had sought medical attention sooner… If only we got a second opinion from another doctor… If only we had tried to be a better person toward them… Secretly, we may make a deal with God or our higher power in an attempt to postpone the inevitable. This is a weaker line of defense to protect us from the painful reality. 4. Depression Two types of depression are associated with mourning. The first one is a
- 9. reaction to practical implications relating to the loss. Sadness and regret predominate this type of depression. We worry about the costs and burial. We worry that, in our grief, we have spent less time with others that depend on us. This phase may be eased by simple clarification and reassurance. We may need a bit of helpful cooperation and a few kind words. The second type of depression is more subtle and, in a sense, perhaps more private. It is our quiet preparation to separate and to bid our loved one farewell. Sometimes all we really need is a hug. 5. Acceptance Reaching this stage of mourning is a gift not afforded to everyone. Death may be sudden and unexpected or we may never see beyond our anger or denial. It is not necessarily a mark of bravery to resist the inevitable and to deny ourselves the opportunity to make our peace. This phase is marked by withdrawal and calm. This is not a period of happiness and must be distinguished from depression. Loved ones that are terminally ill or aging appear to go through a final period of withdrawal. This is by no means a suggestion that they are aware of their own impending death or such, only that physical decline may be sufficient to produce a similar response. Their behavior implies that it is natural to reach a stage at which social interaction is limited. The dignity and grace shown by our dying loved ones may well be their last gift to us. Coping with loss is a ultimately a deeply personal and singular experience — nobody can help you go through it more easily or understand all the emotions that you’re going through. But others can be there for you and help comfort you through this process. The best thing you can do is to allow yourself to feel the grief as it comes over you.
- 10. Resisting it only will prolong the natural process of healing. THE RIGHT TO DIE: To explain 3 the rights to There are legal issues involved in dying. The right to die. Many people Teacher Have min die. do not want to be kept alive by machines or other measures. Consent will Students you ever must be given to do any treatment on a patient. If the patient is not able White discuss will heard to do so, the nearest living relative will be asked. People need to make board rights of understand about their own decisions while they are able.. dying rights of informed individual. dying consent ? The self-determination Act and Obra give a person the right to accept or individual. refuse medical treatment. They also have a right to make advance directives (a written document stating a person’s wishes about health care when the stated person is unable to do so for themselves). Living will (a person’s written statement about the use of life-sustaining measures, feeding tubes, ventilators, and CPR are a few). Durable power of attorney (the power to make decision about health care is given to another person, family or friend, or sometimes a lawyer) These are common forms of advance directives. All health care agencies must inform patients of their right for advance directives on admission. This information must be in writing. The patient’s medical record must have documentation of their advance directives. Do Not Resuscitate Orders… When death is sudden and unexpected, every effort to save life is given. CPR and any and all emergency treatment is given to sustain a person life. Things are different with a long term or chronic illness, the patient has a
- 11. right to have their doctor write a ―No Code," or Do Not Resuscitate DNR order. This means that no attempts will be made to resuscitate a terminally ill person. The person is allowed to die in peace and with dignity. The orders should only be written after the MD speaks with the patient and then with the family, significant others. THE DYING PERSONS BILL OF RIGHTS: Teacher I have a right to- be treated as a living human being until I die transper will ask Students Listout 5 To enlist the ancy questions will the dying min dying persons I have a right to- maintain a sense of hopefulness, however changing its to participate persons bill of rights. focus may be. students. in bill of discussion rights. To be cared for by those who can maintain a sense of hopefulness, . however changing that may be. To express my feelings and emotions about my approaching death, in my own way. To participate in decisions concerning my care. To expect continuing medical and nursing attention even though I have comfort only goals. To Be free from pain! To have my questions answered honestly. Not to be deceived. Have help from my family accepting my death.
- 12. To die in peace and DIGNITY. To retain my individuality and not be judged for my decisions. To discuss and enlarge my religious and spiritual beliefs. To expect the sanctity of my human body will be respected after death. To be cared for by caring, sensitive, knowledgeable people who will attempt to understand my wants and needs, and will gain some sort of satisfaction in helping me face my death. SIGNS OF DEATH : Signs of death or strong indications that a person is no longer alive are: 5 To identify Teacher Students How will min signs of death will will you Cessation of breathing White discuss verbalize assess the Cardiac arrest (No pulse) board with signs of sign of Pallor mortis, paleness which happens in the 15–120 minutes after students. death. death ? death Livor mortis, a settling of the blood in the lower (dependent) portion of the body Algor mortis, the reduction in body temperature following death. This is generally a steady decline until matching ambient temperature Rigor mortis, the limbs of the corpse become stiff (Latin rigor) and difficult to move or manipulate
- 13. Decomposition, the reduction into simpler forms of matter, accompanied by a strong, unpleasant odor CARING FOR THE BODY AFTER DEATH : 10 After the physician has pronounced death and legally documented the min death in the medical record, care of the dead body is usually performed by nurse. An autopsy consent may be requested and obtained , if To enumerate required . if the patient is to be an organ donor ,arrangements will be the purposes made immediately. The family also wishes to view the body before final Teacher Students What and preparation are made. They may be allowed . demons will will interventions tration explain redemonst of care of by rate the dead body. PURPOSES : demonstra procrdure,. The nurse care for the body immediately following death to : tion. - Make the body look as natural and beautiful as possible. - Perform last duty tenderly - Do everything you can for the relatives - Protect other patient from unpleasant sights and sounds which could frighten them. Interventions: The interventions of last offices begin soon after a doctor certifies the cause of death . The practical interventions of last offices provided for the patient are categorised according to hygienic, aesthetic and legal reasons. Although correct compliance with recommended practical procedures for last offices is important, the sensitive and respectful manner of the carer was found to be as important . Respect for a patient's dignity is epitomised by closing the curtain
- 14. around his or her bed immediately after death . Talking to other patients who may have seen the patient die will help allay their fears. No confidential information should be imparted. 1 ) Hygiene Before beginning the last offices the nurse should put on plastic gloves and an apron to reduce the risks of infectious contamination to staff and cross-contamination to patients from body fluids . The main risk of infection is via body fluids , so intravenous devices need to be carefully removed and disposed of. Entrance sites must be covered with a waterproof dressing. Sometimes the body can continue to excrete fluids after death, so pressure should be applied to the lower abdomen to express any residual urine. As further excretion of bodily waste is not expected, the routine packaging of orifices is unnecessary . 2 )Aesthetics Death can alter a patient's appearance, and friends and relatives might find this disturbing. The following course of care is suggested as a means of preparing a patient's body for those who wish to pay their respects and to preserve dignity . This intervention can be justified on the basis that the patient would have adjusted his or her own appearance had he or she been able to. The eyes should be closed with downward pressure and the jaw closed and supported by a bandage tied around the head. This seems a more appropriate and dignified intervention and has less potential to cause harm or leave pressure marks on the patient's face or neck . The patient's dentures should then be removed and cleaned, the inside of the mouth cleaned and the dentures replaced. This ensures that any unpleasant odours are eradicated .
- 15. After undressing, the patient should be given a sponge bath and dressed in according to hospital policy. Bed linen should be removed and replaced with clean sheets, and the bedside area tidied. Dressing the patient in a shroud can make him or her look inappropriate and unnatural. There is no obvious reason that patients should not be dressed in their own, or even in hospital clothes, other than it is not always hospital policy. Next the patient's head should be placed on a pillow and the arms and legs straightened. It has been suggested that laying the arms by the side of the body may cause the hands to blacken, and this would be a concern if relatives wished to hold the deceased's hand later. . Before removal of the body to the mortuary, it should be wrapped tightly in a sheet, to avoid damage during transfer. It is fortunate that other patients do not have to suffer this dehumanising intervention when being transferred by trolley around the hospital; a set of bedrails and a careful porter would seem to suffice. The body is then taken away in a special hospital trolley designed to secrete the body, a protective gesture. 3 )Legal issues The final intervention involves providing a means to easily identify the patient's body and taking an accurate record of all the personal belongings. Attaching hospital identity bands to a patient's wrist and ankle aids identification. A notification of death certificate can also be attached to the sheet in which the patient is wrapped. The certificate should be attached with tape, rather than with a pin, as this may present a hazard to staff handling the body . All personal items should be documented in the patient's property book in the presence of another staff member.
- 16. SUMMARY : 5 Up till now we have discussed about following topics : min Introduction , factors affecting grief and death, meeting the needs of dying person,stages of dying, dying persons bill of rights, signs of death , interventions of dead body including personal hygiene , aesthetics and legal issues. CONCLUSION : 1 min Caring for the dead is a unique aspect of nursing because the deceased will never be aware of it. Although the necessity of providing a high standard of care on the basis of 'upholding and enhancing the good reputation of the professions' is reason enough to provide excellent care, it is respect for the dignity and individuality of all patients . RECAPITULATION : Encourage students to ask questions and to clarify their doubts. 1 ASSIGNMENT : Min Write an assignment on end care of dead body. Date of submission : Student’s Bibliography 1.The trained nurses association of India. New delhi: chandu publication; 2007.p.138 -140. 2.Taylor C. fundamental of nursing. 4th ed. Lippincott: new yourk; p.1079-1089. 3.Barbara Koizer,Glenora Erb,Audrey Jean Berman.Fundamental Of
- 17. Nursing 6th edition. India:Published by Person education;2003.p.822 Teacher’s Bibliography 1.Patricia A. Potter,Anne Grffin Perry.Fundamentals Of Nursing.6th edition.New Delhi : Published by Elsevier;2005.p.390-393 2.Carol Taylor,carol Lillins,Priscilla Le Mone. Fundamental Of Nursing The art and scince of nursing care. 6th edition.Philadelphia:Lippincott publications;2005.p.94-100 3.The Trained Nurses Association of India. Fundamentals Of Nursing 1st edition.New Delhi:Publlished by Secretary-General of TNAI;2005.p.13- 15. 4.Ruth F. Craven.Fundamental Of Nursing.5th edition.Philadelphia: Lippincott Williams & Wilkims Publication;2006.p.89-104
- 18. CENTRAL OBJECTIVE : Caring for the dying and dead illustrates nurses to possess not only practical skills but a knowledge of the professional, ethical and legal factors that are intrinsic to holistic care. SPECIFIC OBJECTIVE : After studying this topic, students will be able to : - list the factors affecting grief and death - analyse and discuss the needs of dying individuals. - enlist the rights of dying individuals. - identify the sign of death - demonstrate the care of the body after death.
- 19. INFORMATION ABOUT CLASS & TEACHER Title of course : B.Sc. Nursing Topic : Death and dying Unit : Level of student : 1st yr B.Sc. nursing No. of student : Date : Time : Venue : Teaching method : Demonstration cum discussion AV AIDS : white board,poster, LCD. Name of evaluator : Mrs. Niru patel Previous knowledge of students :Students are having some knowledge regarding care of dead and dying. INFORMATION ABOUT STUDENT TEACHER Name : Mrs. Mital s. patel
- 20. Year : 1st yr M.Sc.Nursing SANDRA SHROFF ROFEL COLLEGE OF NURSING VAPI SUBJECT – NURSING EDUCATION PRACTICE TEACHING ON DEATH AND DYING SUBMITTED TO: SUBMITTED BY: MRS. NIRU PATEL PATEL MITAL S. ASSISTANT PROFESSER F.Y.M.Sc NSG S.S.R.C.N S.S.R.C.N VAPI VAPI
