This presentation provides an in-depth exploration of compressive neuropathies, a common group of conditions caused by the compression of nerves, leading to symptoms such as pain, numbness, and weakness. We delve into the pathophysiology, common types like carpal tunnel syndrome and sciatica, and the various diagnostic techniques used to identify nerve compression. Additionally, we discuss treatment options ranging from conservative approaches to surgical interventions, as well as strategies for prevention and rehabilitation. Ideal for students, healthcare professionals, and anyone interested in learning about peripheral nerve disorders, this slide deck offers a comprehensive overview of this important neurological condition.






































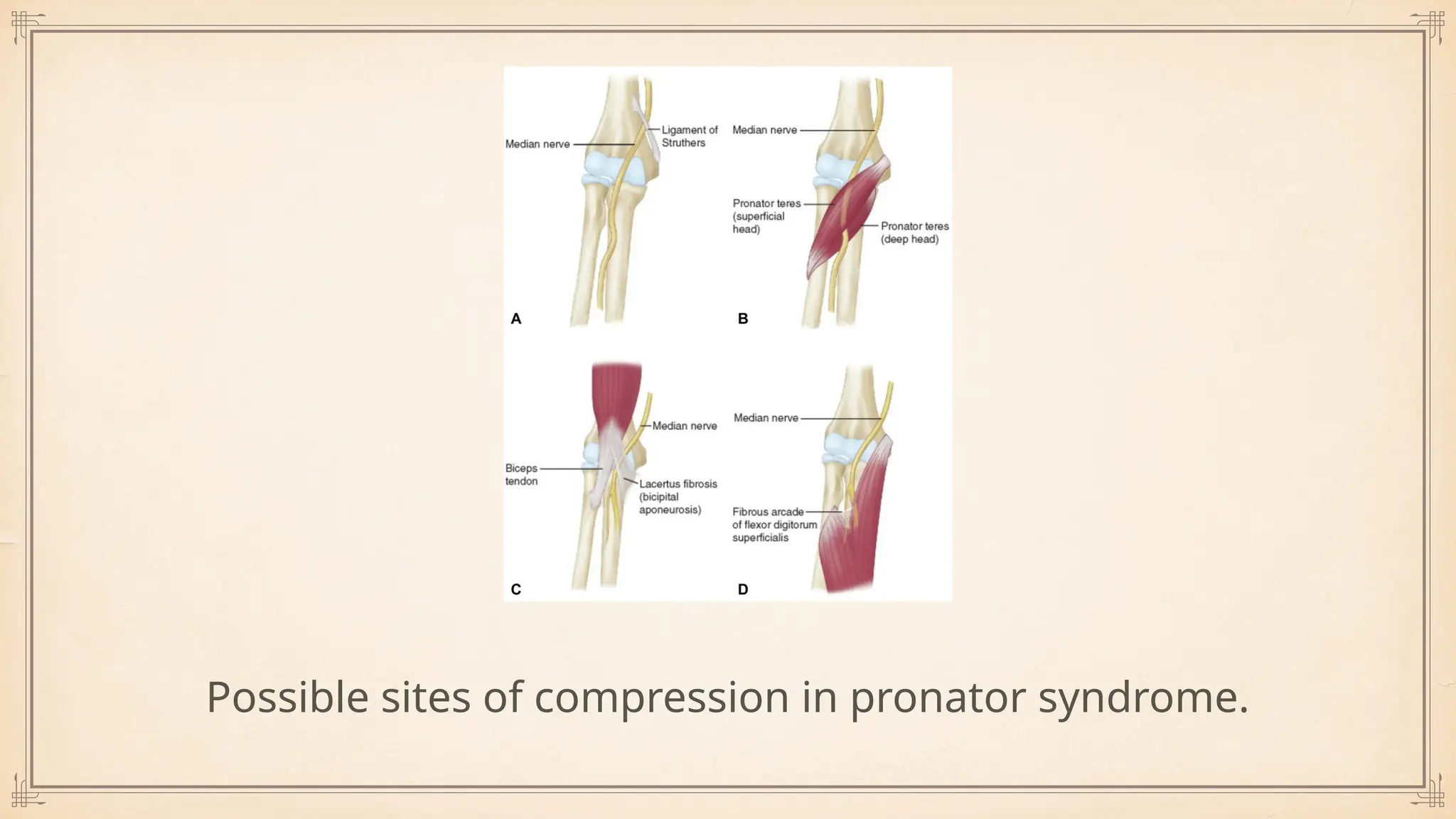









![Causes of entrapment:
Aponeurosis of FCU or b/w FCU heads [ MC site ].
Arcade of struther’s: Formed by an expansion of the medial head of the triceps muscle
that extends to the intermuscular septum[ 2nd MC site ]
Tight fascial band over the cubital tunnel.
Medial head of triceps
Recurrent subluxation of ulnar nerve, results in neuritis.
Osteophytic spurs
Cubitus valgus following supra condylar fracture.](https://image.slidesharecdn.com/compressiveneuropathies-250409172429-b5ced606/75/Compressive-Neuropathies-of-the-Upper-limb-50-2048.jpg)