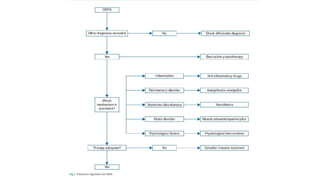
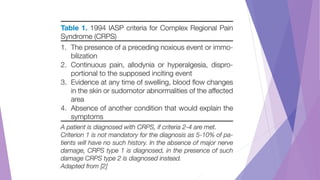
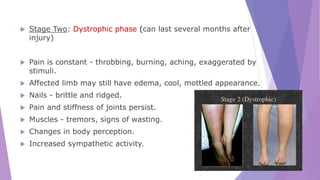
This document discusses Complex Regional Pain Syndrome (CRPS), a neuropathic pain disorder characterized by persistent pain and autonomic features, with two main types: CRPS Type 1 (formerly RSD) and CRPS Type 2 (causalgia). It outlines the condition's historical background, epidemiology, clinical symptoms, pathophysiology, diagnostic criteria, and management strategies, emphasizing the importance of physical and psychological therapy alongside pharmacological treatments. The document also notes risk factors, stages of CRPS, the absence of specific diagnostic tests, and the potential benefits of preventive measures.











![PREVENTION
As treatment options for CRPS are limited, prevention of the
disease would be the best medicine.
Studies have shown supplementation with Vitamin. C
[>500mg/day] initiated immediately after injury or surgery and
continued for 45-50 days helped to reduce the risk of CRPS.](https://image.slidesharecdn.com/complexregionalpainsyndromeautosaved-240617174113-5512c3fe/85/COMPLEX-REGIONAL-PAIN-SYNDROME-Autosaved-pptx-28-320.jpg)