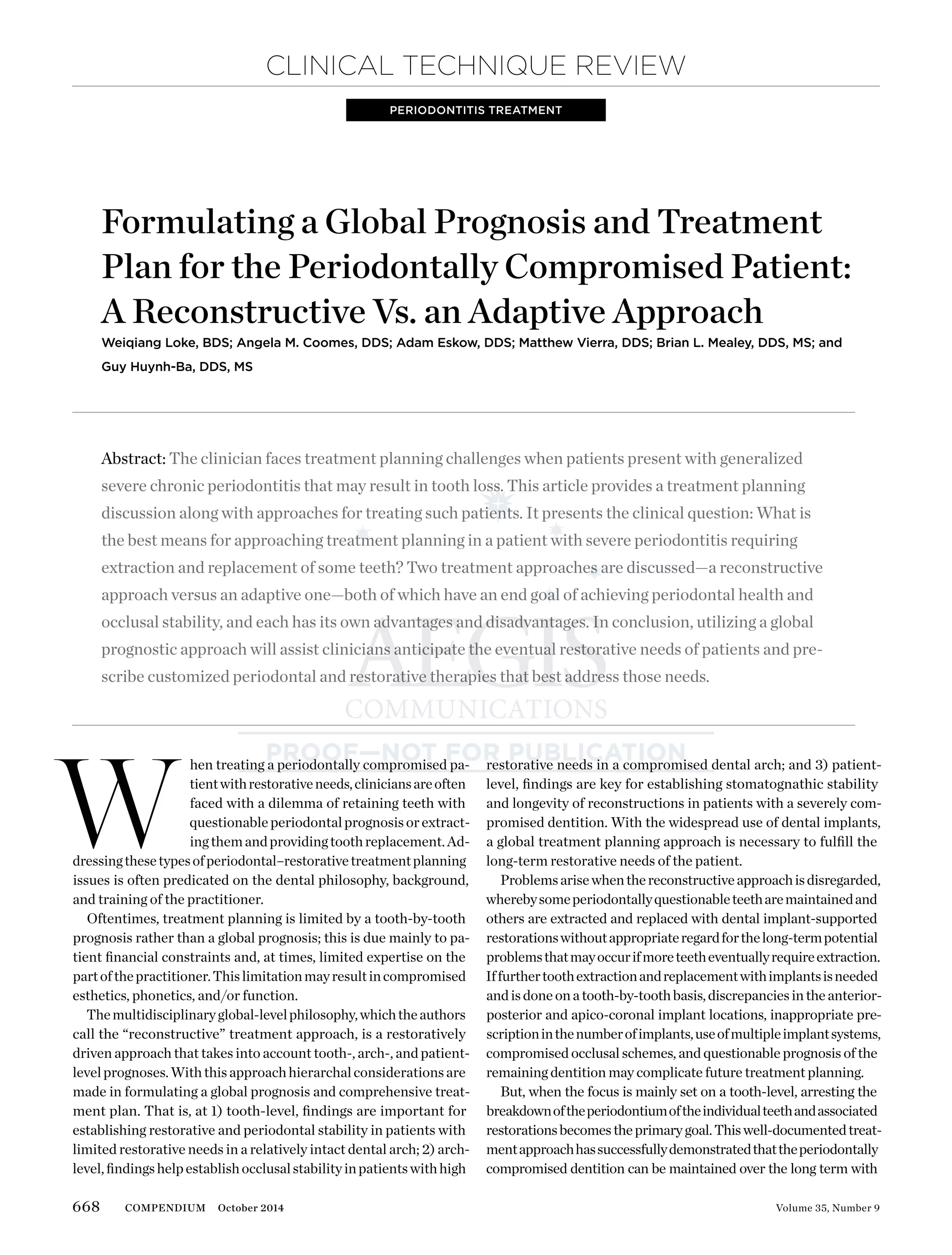
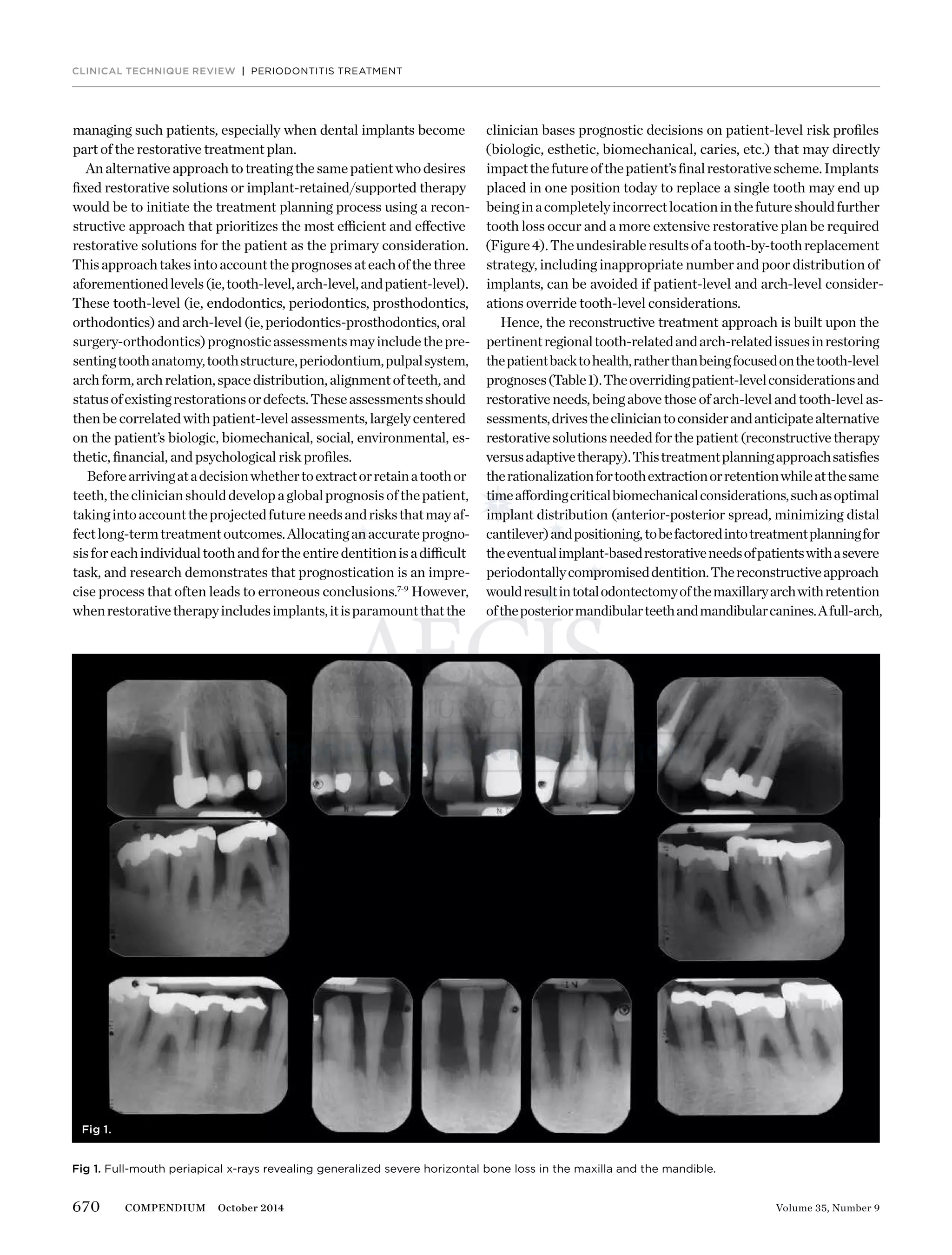
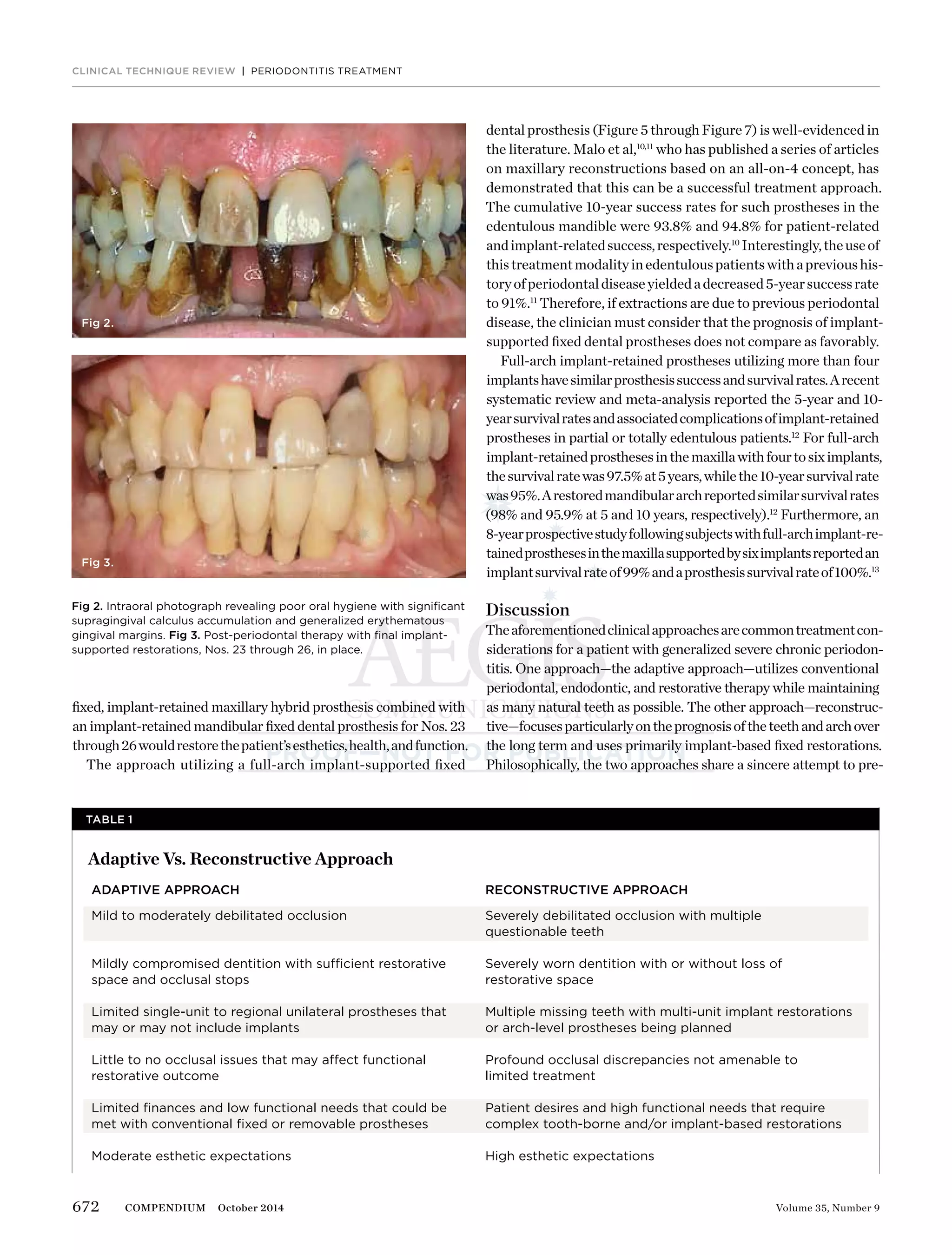
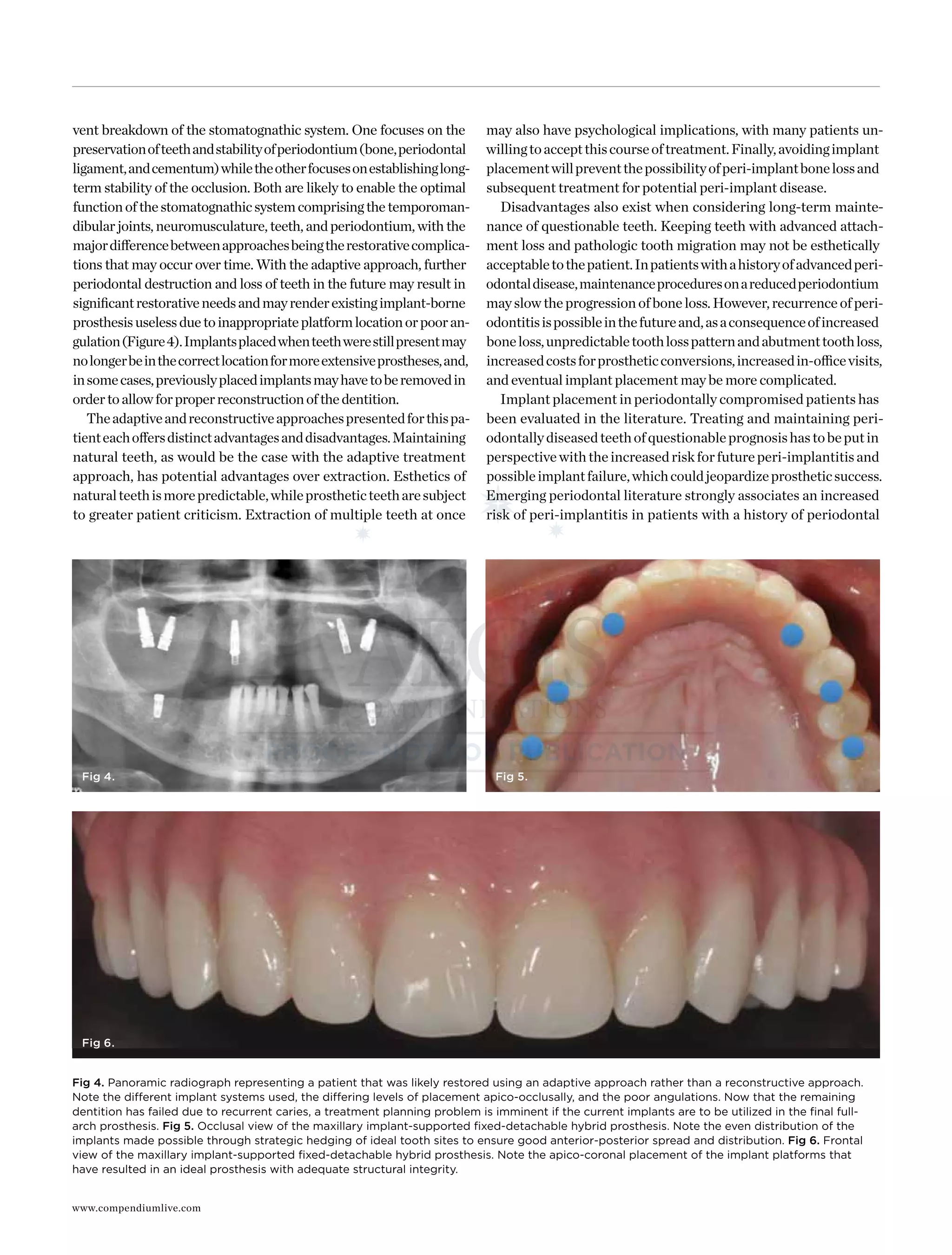
The document discusses two approaches to treatment planning for patients with severe periodontitis - a reconstructive approach and an adaptive approach. The reconstructive approach favors early extraction of questionable teeth to place dental implants, while the adaptive approach aims to retain natural teeth through nonsurgical and surgical periodontal therapy. The case study presented illustrates an adaptive approach, where periodontally hopeless teeth were extracted but other teeth were retained through nonsurgical therapy, surgery, and periodic maintenance. Over time, some retained teeth were later extracted and replaced with implants due to increased mobility.