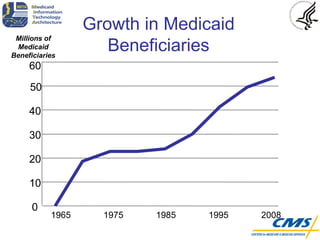
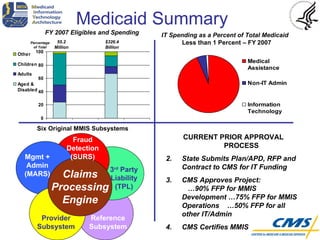
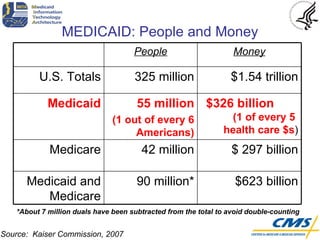
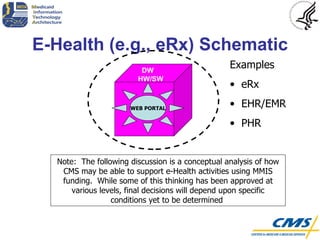
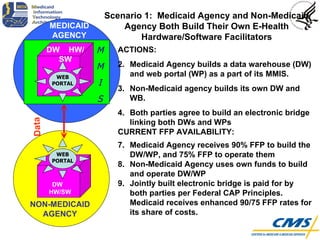
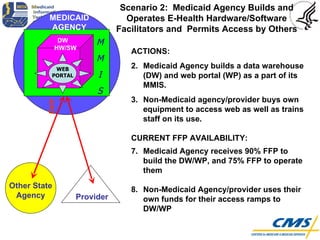
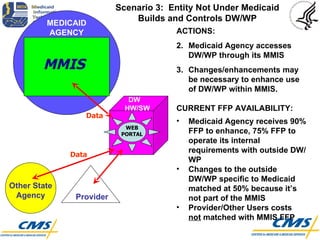
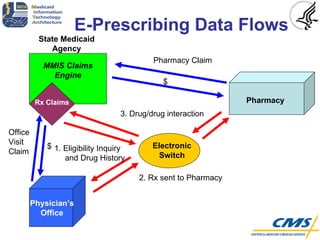
The document discusses Medicaid IT architecture and interoperability. It provides background on Medicaid spending and beneficiaries. It then describes the Medicaid IT Architecture (MITA) framework, which aims to make Medicaid systems more patient-centric, interoperable, and based on industry standards. The framework is a roadmap to guide states in building their own customized IT solutions over 5-10 years. Finally, the document discusses three scenarios for funding collaborative environments and electronic health initiatives like e-prescribing through the existing Medicaid Management Information System (MMIS) funding structure.