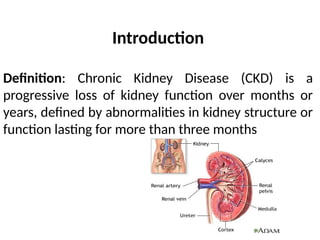
Chronic kidney disease (CKD) is a progressive loss of kidney function affecting about 10% of the global population, primarily due to diabetes and hypertension. It progresses through five stages based on glomerular filtration rate (GFR), with various clinical features and complications arising in later stages. Management includes lifestyle modifications, medical therapy for complications, and renal replacement options like dialysis and transplantation.