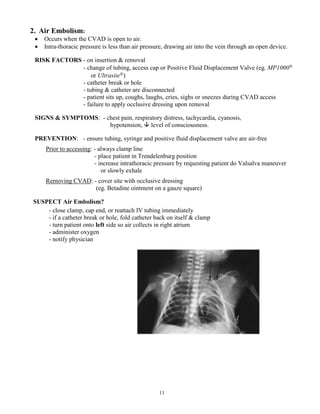
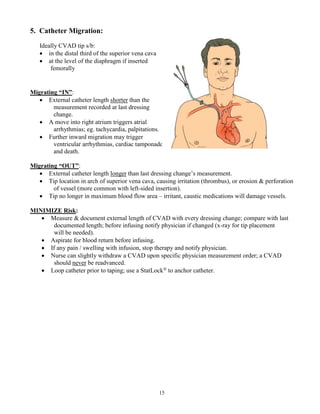
The document serves as a comprehensive learning guide on central venous access devices (CVADs), detailing device designs, types, and associated risks and complications. It outlines the educational objectives for nursing competencies related to CVAD care, including procedures for insertion, maintenance, and recognizing potential issues. Key information includes types of CVADs—non-tunneled, PICC, tunneled, and totally implanted—along with risks such as infection and catheter occlusion, and actions for effective management.