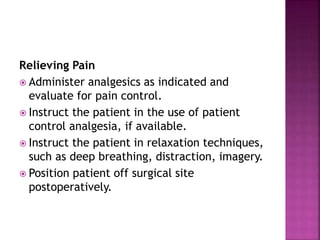
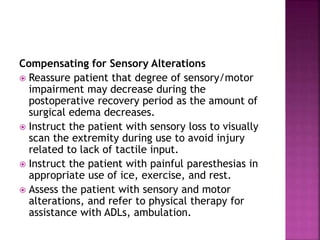
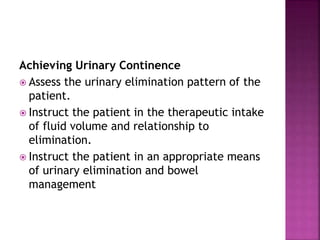
This document discusses intracranial neoplasms (brain tumors). It notes that brain tumors can originate in the central nervous system or metastasize from other sites. Symptoms vary depending on the location of the tumor in the brain and can include headaches, vomiting, seizures, and neurological deficits. Diagnostic testing includes imaging like CT scans and MRI. Treatment aims to relieve increased intracranial pressure and neurological deficits but can result in further deficits or death. Nursing care focuses on pain management, prevention of injury, reducing anxiety, optimizing nutrition, and supporting family coping.
![ Brain stem: dysphagia, incontinence, cardiovascular
instability, respiratory depression, coma, cranial
nerve dysfunction
Hypothalamus: loss of temperature control, diabetes
insipidus, SIADH
Pituitary/sella turcica: visual field deficits,
amenorrhea, galactorrhea, impotence, cushingoid
symptoms, elevated growth hormone,
panhypopituitarism
Referred symptoms (related to the vasogenic
[extracellular] edema of the tumor presence):
usually present symptoms of ischemia of region
distal to the actual lesion.
Seizures.](https://image.slidesharecdn.com/16-240222181136-70f8a59e/85/CENTRAL-NERVOUS-SYSTEM-TUMORS-nursing-care-process-5-320.jpg)